Is there a long-term survival benefit with on pump coronary artery bypass grafting?
A simple choice?
Coronary artery bypass grafting (CABG) has become the gold standard of care for the treatment of coronary artery disease involving multiple vessels (1). This involves a choice as to whether to perform the surgery on (with cardiopulmonary bypass, CPB) or off pump (on the beating heart, without CPB). Each technique has its advantages and disadvantages. On pump surgery provides a motionless operative field, but can be associated with a number of complications including myocardial ischemic injury, coagulation disorders, neurocognitive deficits, strokes and a systemic inflammatory response (2). In contrast off pump surgery avoids aortic manipulation and, although more technically demanding (2), has been helped by the invention of stabilizing devices (3). The debate as to which approach is superior has been raging for over 40 years. Indeed, an excellent example of the division in opinion is the conduct of 90% of CABG off pump in India (2) compared to only 20% worldwide (4) and 13% in the US and Canada (5).
Evidence from meta-analyses
By 2012, 86 randomized controlled trials (RCTs) had been completed comparing off vs. on pump CABG. This enabled the completion of a Cochrane review on the subject (6). This is one of the largest meta-analyses to date, probably because a range of follow-up times was investigated, whereas three recent meta-analyses, completed in 2016 (7-9), concentrated on short-term outcomes only. The results of the Cochrane review revealed no significant differences in the occurrence of myocardial infarction, re-intervention and renal insufficiency. One analysis, which definitely favoured off-pump was the incidence of atrial fibrillation, where the risk ratio (RR) was 0.78 [95% confidence interval (CI): 0.63–0.96; I2=67%; Z=2.29; P=0.02] (6). Off-pump was also favoured if the fixed effect model was used for the stroke analysis (P=0.04), although this difference disappeared in the random effects model. Undoubtedly, though the most striking result concerned mortality. The pooled analysis of all RCTs reporting mortality produced an RR of 1.24 (95% CI: 1.01–1.53; I2=0%; Z=2.04; P=0.04) favouring on pump (6). In trials that the authors considered to be low risk of bias trial sequential analysis revealed a 30% higher risk of mortality in the off pump group. Further analysis showed the number needed to harm was 67. Subgroup analysis comparing trials with <30 days’ follow-up with those with >30 days’ follow-up demonstrated that the group responsible for the significant results favouring on pump came from the studies with the longer follow-up. It should be noted though that length of follow-up in the >30 days’ subgroup varied widely from 2 months to 5 years (6).
A significant limitation of the Cochrane review was that many of the trials were underpowered. Of the 86 included RCTs, only 25 involved >100 participants and only two RCTs included >500 participants (DOORS and ROOBY) (5,10). This may have contributed to the authors’ conclusion that only 10 RCTs were at low risk of bias. Nevertheless, the analysis of the low risk of bias RCTs supported the result concerning mortality (RR 1.35; 95% CI: 1.05–1.7; I2=0%; Z=2.51; P=0.01) (6). Other limitations noted by the authors concerned the lack of patients with triple vessel disease and those at high risk. At the time of the Cochrane review the most recent published results they were able to include came from 2011. Since that time, several more RCTs have been published including 2 of the largest to date (CORONARY and GOPCABE) (11,12). These additional RCTs prompted the completion of 3 further meta-analyses in 2016.
The largest meta-analysis to date was conducted by Kowalewski et al. (7). This meta-analysis is also unique for its inclusion of meta-regression analysis where the log OR of the Off pump group was plotted against the OR of the control (on pump) group, using the inverse of the log variance as weight. This enabled the authors to investigate the effect of risk. The forest plots revealed no significant difference in the occurrence of mortality or MI, whilst in the case of stroke the off pump group was significantly favoured. The results of the meta-regression suggested that outcomes may be related to the patient’s risk profile and that performing surgery off pump may be preferable in high risk patients. It should be noted that this represents only one method for assessing the impact of a patient’s risk profile, other parameters such as age, EUROscore, ejection fraction and the presence of pulmonary disease may also be worth investigating. The other two meta-analyses published in 2016 produced conflicting results (8,9). The results of Deppe et al. (8) concur with those of Kowalewski et al. (7) with regard to the significant advantage of off pump with respect to stroke, whereas Dieberg et al. (9) found no difference perhaps because they included more studies than Deppe et al. (8). Dieberg et al. did, however find off pump to be significantly favoured with respect to atrial fibrillation (9).
Thus the results of these meta-analyses so far conducted are contradictory, concentrate largely on short-term outcomes and include many small (<100 participants) studies. It is worth mentioning two further meta-analyses in this section, because they attempted to investigate longer-term outcomes, although longer-term in these cases means either 1-year of follow-up or anything over 6 months. One of these studies used inclusion criteria, which excluded participants with a mean age <60 years (13). As a consequence, only 4 so-called long term studies were included [GOPCABE (1-year) (12); DOORS (6-months) (10); CORONARY (1-year) (14) and Møller (3-year) (15)] and significant RCTs including Angelini et al. (4) were missed. In this small comparison there were no differences in the incidences of stroke, MI and mortality (13). In contrast, the meta-analysis investigating 1-year outcomes significantly favoured the on pump group with regard to mortality (16), which correlates with the results of the Cochrane review (6).
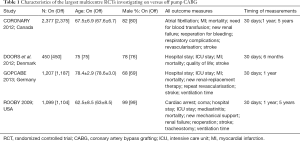
Can the large clinical trials provide clarity? Short-term outcomes
Confused? The evidence from the meta-analyses is contradictory and plagued by underpowered RCTs. There are only 4 multicentre RCTs investigating on vs. off pump CABG, which included >500 participants. These are CORONARY (11), DOORS (10), GOPCABE (12) and ROOBY (17) (Table 1). At 30 days after surgery all of these RCTs showed an insignificant difference between the on and off pump groups for mortality and stroke. CORONARY (11), DOORS (10) and GOPCABE (12) showed no difference in the incidence of MI and CORONARY (11), GOPCABE (12) and ROOBY (17) showed no difference in new onset renal failure. At this early time point the most worrying aspect concerned the completeness of revascularization, because compared to the on pump group repeat revascularization was significantly greater in the off pump group in CORONARY (11) and DOORS (10) and the number of grafts performed vs. those planned in the off pump group was significantly lower in ROOBY (17). In summary at this early time point there were no differences in hard clinical outcomes, although there was a question about the completeness of the revascularization in the off pump group.
Full table
Mid-term outcomes
The RCT with the shortest follow-up was DOORS (10), which only investigated mortality at 6 months, finding no difference between the groups. The other three studies reported 1-year outcomes. CORONARY (11) continued to investigate a composite composed of death, MI, stroke and new renal failure requiring dialysis for which there was no difference between the two groups. Although there had been the initial difference at 30 days in the rate of repeat revascularisation, it would be stretching the point too far to say there was still a trend towards an increased rate of repeat revascularization in the off pump group, as the P value was 0.07. These results are very similar to the GOPCABE group (12), who also found no differences in the rate of death, MI, stroke and new renal replacement therapy. In GOPCABE’s case there was no uncertainty, there was definitely no difference in the rate of repeat revascularization between the groups. There was also no difference in repeat revascularization rate at 1-year in the ROOBY RCT (17). However, in contrast to the foregoing discussion, there was a significant difference in the 1-year composite (death, nonfatal MI and repeat revascularization) in the ROOBY RCT. Here the on pump appeared to be favoured with the underlying reason possibly due to a significantly lower number of deaths from cardiac causes (2.7% off pump; 1.3% on pump; P=0.03), although there was no significant difference in the Kaplan Meier curves (17). Also noteworthy from the 1-year follow-up of the ROOBY RCT is the significantly lower rate of graft patency in the off pump group. This was especially marked for saphenous vein grafts and when the left internal thoracic was grafted to the left anterior descending artery (17).
Long-term outcomes
Perhaps the ultimate test of the efficacy of on or off pump CABG is patient freedom from cardiovascular events in the long term. This year has witnessed the landmark publication of the 5-year outcomes of the CORONARY (18) and most recently ROOBY (5) trials. The message from the CORONARY (18) trial continued to be no significant differences in the rate of death, MI, stroke, new renal failure requiring dialysis, cost and quality of life. However, in view of the results at 1-year follow-up which began to favour the on pump group, it was of some significance when the 5-year outcomes of the ROOBY RCT (5) became available and the findings if you are an on pump supporter did not disappoint. The primary outcomes investigated were death from any cause and MACE (composite of death from any cause, repeat revascularization or nonfatal MI). Time to event was also recorded. Secondary outcomes included 5-year rate of death from cardiac causes, repeat revascularization, nonfatal MI and the impact of the surgeon’s experience. The 5-year rate of death was 15.2% in the off pump group compared to only 11.9% in the on pump group (P=0.02) giving rise to a hazard ratio for death in the off pump compared to on pump group of 1.3 (95% CI: 1.04–1.64; P=0.02) (5). This translates into a significant 28% higher risk of death from any cause after off pump CABG. There is an interesting symmetry between this and the Cochrane review (6) with respect to mortality. None of the secondary outcomes showed any significant difference and there was no significant difference based on the surgeon’s experience.
Is there a long-term survival benefit with on pump?
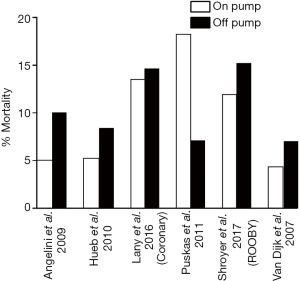
The 5-year results from the ROOBY RCT (5) suggested that there was a long-term survival advantage associated with on pump CABG compared to off pump. Is there any other evidence to support this? A total of 6 RCTs have reported over 4 years of outcomes including and in addition to CORONARY (18) and ROOBY (5): Angelini et al. (4); Hueb et al. (19); Puskas et al. (3) and van Dijk et al. (20). Figure 1 compares the incidence of mortality in the on and off pump group in each of these studies. In all of these studies bar one (3) the numbers that had died by the follow-up point were larger in the off pump group compared to the on pump group (4,5,18-20). In the exception, Puskas et al. (3), although there was a significant difference at the 5-year follow up point, this had disappeared by 7 years. Thus far the ROOBY (5) trial is the only trial to report a significant difference in favour of the on pump group at 5 years, though it should be noted that Angelini et al. (4) do not state the P value in their study where mortality was double that of the on pump group in the off pump group. The ROOBY (5) trial authors do note that their participants tended to have slightly higher rates of hypertension, peripheral vascular disease and atrial fibrillation than the CORONARY (11) trial, whilst there were lower rates of urgent status, diabetes and female sex.
Conclusions
Although CABG remains a gold standard choice of treatment for triple vessel coronary artery disease, the opinion as to whether this should be performed off or on pump is divided. Evidence from meta-analyses has been contradictory and overshadowed by the low numbers of participants in many of the trials. Of the four large trials that have been carried out, three have consistently showed no differences in hard clinical outcomes (death, rate of MI, stroke and new renal failure) (10-12). In addition, any early advantages in terms of completeness of revascularization in the on pump group have disappeared by the mid-term follow up. The one exception to this is the ROOBY (5) trial, which has shown at both the mid-term and long-term follow-up points a significant difference favouring on pump with regards to mortality. Perhaps the results of this one, albeit large clinical trial, are insufficient to come to a definitive conclusion; however, they do support the notion that on pump CABG is non-inferior to off pump CABG and may even in certain patients be beneficial. The next question is identifying precisely who those patients are.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Fudulu D, Benedetto U, Pecchinenda GG, et al. Current outcomes of off-pump versus on-pump coronary artery bypass grafting: evidence from randomized controlled trials. J Thorac Dis 2016;8:S758-71. [Crossref] [PubMed]
- Apostolakis E, Papakonstantinou NA, Koniari I. Myocardial revascularization without extracorporeal circulation: why hasn’t it convinced yet? Ann Card Anaesth 2017;20:219-25. [Crossref] [PubMed]
- Puskas JD, Williams WH, O’Donnell R, et al. Off-pump and on-pump coronary artery bypass grafting are associated with similar graft patency, myocardial ischemia, and freedom from reintervention: long-term follow-up of a randomized trial. Ann Thorac Surg 2011;91:1836-42. [Crossref] [PubMed]
- Angelini GD, Culliford L, Smith DK, et al. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long-term follow-up of 2 randomized controlled trials. J Thorac Cardiovasc Surg 2009;137:295-303. [Crossref] [PubMed]
- Shroyer AL, Hattler B, Wagner TH. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med 2017;377:623-32. [Crossref] [PubMed]
- Møller CH, Penninga L, Wetterslev J, et al. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev 2012.CD007224. [PubMed]
- Kowalewski M, Pawliszak W, Malvindi PG, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: meta-analysis. J Thorac Cardiovasc Surg 2016;151:60-77. [Crossref] [PubMed]
- Deppe AC, Arbash W, Kuhn EW, et al. Current evidence of coronary artery bypass grafting off-pump versus on-pump: a systematic review with meta-analysis of over 16,900 patients investigated in randomized controlled clinical trials. Eur J Cardiothorac Surg 2016;49:1031-41. [Crossref] [PubMed]
- Dieberg G, Smart NA, King N. On- vs. off-pump coronary artery bypass grafting: a systematic review and meta-analysis. Int J Cardiol 2016;223:201-11. [Crossref] [PubMed]
- Houlind K, Kjeldsen BJ, Madsen SN, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients. Results from the Danish On-pump versus Off-pump randomization study. Circulation 2012;125:2431-9. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 2012;366:1489-97. [Crossref] [PubMed]
- Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Eng J Med 2013;368:1189-98. [Crossref] [PubMed]
- Luo T, Ni Y. Short-term and long-term postoperative safety of off-pump versus on-pump coronary artery bypass grafting for coronary heart disease: a meta-analysis for randomised controlled trials. Thorac Cardiovasc Surg 2015;63:319-27. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013;368:1179-88. [Crossref] [PubMed]
- Møller CH, Perko MJ, Lundt JT, et al. Three year follow-up in a subset of high-risk patients randomly assigned to off-pump versus on-pump coronary artery bypass surgery: the Best Bypass Surgery Trial. Heart 2011;97:907-13. [Crossref] [PubMed]
- Zhang B, Zhou J, Li H, et al. Off-pump coronary artery bypass grafting does not increase the 1-year mortality compared to on-pump: a meta-analysis of randomized controlled trials. Int J Cardiol 2013;169:e93-5. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 2016;375:2359-68. [Crossref] [PubMed]
- Hueb W, Lopes NH, Pereira AC, et al. Five-year follow-up of a randomized comparison between off-pump and on-pump stable multivessel coronary artery bypass grafting. The MASS III trial. Circulation 2010;122:S48-52. [Crossref] [PubMed]
- van Dijk D, Spoor M, Hijman R, et al. Cognitive and cardiac outcomes 5 years after off-pump vs on-pump coronary artery bypass graft surgery. JAMA 2007;297:701-8. [Crossref] [PubMed]


