Prioritizing molecular markers to test for in the initial workup of advanced non-small cell lung cancer: wants versus needs
Introduction
Among the many ongoing developments in management of advanced non-small cell lung cancer (NSCLC), one of the leading ones is the dynamic nature of the initial workup, specifically which molecular markers should be considered a standard of care to seek and detect. This is dependent in part on a tumor’s specific histologic breakdown, as the molecular drivers most clearly associated with effective targeted therapies are far more common in patients with advanced lung adenocarcinoma or at least non-squamous subtypes, leading to different recommendations for squamous vs. non-squamous advanced NSCLC. The core question that frames the recommendations for what should constitute the initial molecular marker evaluation is whether there is sufficient evidence to warrant widespread screening for the marker and whether not only detecting it but detecting it during the initial workup confers a significant efficacy benefit for the patient.
Guidelines on NSCLC from the National Comprehensive Cancer Network (NCCN) include a growing table of molecular markers for which the data supporting commercially available treatments not approved for that specific target in advanced NSCLC arguably warrant treatment outside of a trial setting, particularly if a clinical trial for the marker in question is inaccessible to a patient (1). Today, the list of identified mutations reported in a patient’s genomic panel from their tumor is often accompanied by suggested treatment options that may include a subset supported by randomized trials alongside others with far more limited phase I or II data, and even still others for which only preclinical data are offered as a speculative option to consider. In this scenario, it becomes critical for clinical oncologists to weigh the depth and quality of the evidence compared to well-established, standard treatment options.
At the present time, only a very limited subset of markers truly reach a threshold of sufficient evidence to displace competing standard first line treatment options. Those include activating mutations in the epidermal growth factor receptor (EGFR) gene, as well as translocations in the anaplastic lymphoma kinase (ALK) or ROS1 proto-oncogene receptor tyrosine kinase (ROS1) genes. This list is likely to grow over time, as new markers are identified and new data generated that demonstrate higher efficacy than could be anticipated from other first line treatment options. Nevertheless, it is important for clinical oncologists to avoid putting too fine a point on limited data with rare mutations, instead prioritizing the potential targeted therapy options according to the quality and quantity of evidence for each potential marker. We will now review why EGFR, ALK, and ROS1 have emerged as the markers that merit highest priority, based on the available evidence at this time, for detection in the initial workup of patients with advanced non-squamous NSCLC.
EGFR
EGFR inhibitors as a targeted therapy were initially developed prior to the discovery of EGFR mutations in 2004 (2,3). Initially, gefitinib and then erlotinib were administered to a broad population of patients, predominantly patients previously treated with one or more lines of systemic therapy (nearly invariably conventional chemotherapy, as the only established treatment approach for advanced NSCLC). First gefitinib (4) and then erlotinib (5) were FDA approved for unselected patients who had received prior chemotherapy. Erlotinib was approved for a broad population based on the overall survival (OS) benefit seen in the BR.21 trial that randomized patients 2:1 between erlotinib and best supportive care (BSC) (6). The FDA subsequently limited this agent to those not starting it as a new therapy (7) after the ISEL trial failed to demonstrate an improvement in a similar trial of unselected patients randomized between gefitinib and BSC (8).
Investigators and clinical oncologists readily identified that patients with certain clinical and/or histologic characteristics were far more likely to respond well to gefitinib (9) or erlotinib (10). Asians, women, never-smokers, and those patients with adenocarcinoma histology and especially bronchioloalveolar carcinoma histology, as it was known at that time, prior to a revision of the classification of lung adenocarcinoma pathology (11), were consistently associated with a higher probability of a dramatic and often prolonged response to EGFR TKIs (9,10). Even after the identification of mutations in the EGFR gene commonly seen in patients with strong responses to EGFR TKIs were found to be enriched in patients with these clinical features (2,3,12), it remained debatable whether molecular selection is incrementally more valuable than clinical selection of patients most likely to benefit from these agents.
The value of molecular selection as an alternative to clinical selection was illustrated definitively in a post-hoc analysis of the IPASS trial that randomized 1,217 Asian patients with an advanced lung adenocarcinoma and/or a minimal prior smoking history (94% never-smokers) to either standard carboplatin/paclitaxel or gefitinib as first line therapy (13). The trial met its primary objective of non-inferiority of gefitinib relative to chemotherapy, actually superiority in the primary endpoint of progression-free survival (PFS) [hazard ratio (HR) 0.74, P<0.001]. The most clinically significant finding came from the post hoc analysis of approximately 1/3 of the enrolled patients who had tissue available for molecular testing demonstrated remarkably different results in the 60% of patients with an EGFR mutation compared with the 40% who did not. Specifically, this analysis revealed that these two populations demonstrated remarkably different efficacy with gefitinib relative to chemotherapy, such that those with an identified EGFR mutation experienced a significantly longer PFS with gefitinib than with carboplatin/paclitaxel (HR 0.48, P<0.001) while the opposite was true for the patients without an EGFR mutation (HR 2.85, P<0.001). Similarly, the response rate was significantly higher with gefitinib than with chemotherapy for those patients with an EGFR mutation (71.2% vs. 47.3% for gefitinib vs. chemotherapy, respectively), while the opposite was true for patients who were EGFR mutation-negative (23.5% vs. 1.1% for chemotherapy vs. gefitinib, respectively). In summary, even among never-smoking Asian patients with a lung adenocarcinoma, the benefit of an EGFR TKI was associated overwhelmingly with the presence of an EGFR mutation. Without it, patients fare far worse with first line gefitinib, highlighting that unselected/incorrectly selected patients can be harmed by starting treatment with first-line EGFR TKI therapy instead of chemotherapy.
Another trial that highlighted the potentially detrimental effect of administering first line EGFR TKI therapy to an unselected population was the European TORCH trial (14), which randomized previously untreated patients to either cisplatin/gemcitabine chemotherapy followed by erlotinib upon progression or to erlotinib first line followed by cisplatin/gemcitabine upon progression. This trial was terminated early after the Independent Data Monitoring Committee observed a significantly worse PFS and also OS in those patients assigned to first line erlotinib. These findings underscored the potential harm of administering an EGFR TKI first line to a population of patients who, without molecular selection, should be presumed to fare significantly better with conventional chemotherapy as initial treatment.
Over the ensuing few years, multiple randomized trials of molecularly selected patients with EGFR mutations were conducted, testing first line EGFR TKI vs. chemotherapy. These studies, whether testing gefitinib (15,16), erlotinib (17,18) or afatinib (19,20) in Asia or other parts of the world, have produced overall quite consistent results that are summarized in Table 1. Notably, several were stopped early, after an interim analysis demonstrated highly significant differences favoring the EGFR TKI arm, leading to termination of study randomization and, in general, high crossover from chemotherapy to EGFR TKI therapy. Overall, these studies reveal a theme of highly superior response rates and PFS in the arm receiving an EGFR TKI, relative to conventional chemotherapy, though without a significant difference in OS. With median PFS typically in the range of one year, it is overwhelmingly likely that these EGFR TKis confer a significant survival benefit that is difficult to measure in trials in which the overwhelming majority of patients not started on initial EGFR TKI therapy cross over to receive it later. The fact that EGFR mutation-positive patients have been shown to live significantly longer in the era after introduction of EGFR TKIs (21) provides compelling evidence that this class of agents improves OS, even if it is unethical to withhold such an effective therapy now in order to prove that point.
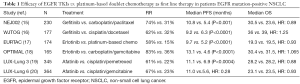
Full table
The absence of an OS benefit has been widely attributed to the high crossover of patients from chemotherapy to EGFR TKI therapy upon progression. Though an analysis of pooled results from the LUX-Lung 3 and LUX-Lung 6 trials reported a significant OS benefit among patients with an EGFR exon 19 deletion (22) the significance of this finding remains unclear. Notably, the LUX-Lung 7 trial that directly compared afatinib to gefitinib (23), which has not demonstrated a survival benefit relative to chemotherapy in EGFR mutation-positive patients, revealed a significantly prolonged PFS but failed to demonstrate a superior OS with afatinib. Notably, the results of LUX-Lung 7 did not indicate any differentially greater activity of afatinib in patients with an exon 19 deletion compared to those patients with an EGFR L858R substitution. These results call into question the validity of the findings of the post hoc analysis of the pooled results of the LUX-Lung 3 and LUX-Lung 6 trials.
Over the course of these trials of EGFR mutation-positive patients receiving EGFR TKIs or chemotherapy, it also became clear that the favorable results consistently seen with EGFR TKIs applies to the 88–90% of patients with either of the common, “activating” mutations, specifically an exon 19 deletion or L858R substitution on exon 21 of the EGFR gene (24,25). In contrast, a few specific subtypes such as G719x and L861Q may be associated with favorable responses, while others, such as most exon 20 insertions, are very unlikely to respond (24,25). The approved EGFR TKIs are specifically indicated for patients with the common, activating mutations (26-28).
Taken together, the extensive trials of EGFR TKIs in broad, unselected advanced NSCLC populations and others focused on patients with activating EGFR mutation-positive patients produce several clear conclusions. First, patients whose tumors don’t harbor an activating EGFR mutation do significantly worse with initial EGFR TKI therapy than with chemotherapy-based treatment. Second, those patients with an EGFR mutation-positive cancer consistently demonstrate a superior RR and PFS with any of the EGFR TKIs in wide use. While a survival benefit with afatinib has been identified in a post hoc analysis of pooled trial results, it has not demonstrated a survival benefit in a head to head trial with another EGFR TKI. With the current FDA approval for all of the EGFR TKIs currently limited to patients with a known activating EGFR mutation, testing for this marker is the only means by which this significant minority of patients can receive the prolonged PFS and almost certainly significantly improved OS that can be delivered by EGFR TKI therapy.
It may arguably be stated that there is no clear evidence demonstrating that it is incontrovertibly better to administer EGFR TKI therapy as first line treatment, as it has been shown that EGFR TKIs have overall comparable efficacy if administered as a later line of therapy (9). Nevertheless, the crossover rate to EGFR TKI therapy in the various first line trials of EGFR TKIs vs. chemotherapy invariably falls short of 100% of patients, even those whose tumor harbors a known EGFR mutation who receive first line chemotherapy on a trial; depending on the rate of clinical progression and the practical limitations of the health care system, a significant fraction of patients may miss that opportunity. Given the overall far more favorable therapeutic index of EGFR TKIs than chemotherapy, as well as the greater efficacy of EGFR TKIs in the central nervous system (29), EGFR TKI therapy emerges as the optimal first line patients in whom an activating EGFR mutation has been identified. Whether a third generation EGFR TKI such as osimertinib should be favored as first-line therapy over gefitinib or erlotinib for patients with an activating mutation is the focus of the FLAURA trial (30). This study has been reported as positive for its primary endpoint of PFS (31), though it is presently unknown whether the magnitude of the difference will be sufficient to make it a new standard of care, particularly as osimertinib is a current appealing second-line option for patients with progression on gefitinib, erlotinib, or afatinib and whose cancer harbors the EGFR acquired resistance mutation T790M (32), as seen in approximately 50–60% of cases of acquired resistance to one of these agents (33).
ALK
ALK rearrangements were first identified in NSCLC tumors several years after discovery of the EGFR mutations (34), with potentially active ALK inhibitors following very shortly thereafter. Noted in initial series to be present in approximately 4% of NSCLC tumors, and disproportionately in younger never-smokers with an adenocarcinoma (35) ALK rearrangements in cell lines were subject to inhibition by ALK inhibitors that were readily brought into clinical development. Crizotinib, in development at the time largely as a MET inhibitor but also noted to have activity as an ALK inhibitor (36), was the subject of a phase I/II study that ultimately enrolled 82 patients (out of approximately 1,500 screened), demonstrating a RR of 57% and an estimated 6 month PFS of 72% (37), leading to the accelerated approval of crizotinib for ALK-positive NSCLC in 2011 (38). This approval generated a second detectable molecular alteration, in a similar patient population as that in which EGFR mutations are most commonly identified, for whom a commercially available and highly efficacious targeted therapy was available.
With a RR and PFS so clearly superior to that expected for standard chemotherapy, many in the US began testing routinely for ALK rearrangements in addition to EGFR mutations, in anticipation of favoring crizotinib as a first line therapy. Definitive evidence of the superior efficacy of crizotinib over chemotherapy in ALK-positive patients would follow with the results of the PROFILE 1014 trial (39), which demonstrated a significantly superior PFS (median 10.9 vs. 7.0 months, HR =0.45, P<0.001) and RR (74% vs. 45%, P<0.001). As was the case in trials of EGFR TKIs vs. chemotherapy as first line therapy, PROFILE 1014 did not demonstrate a significant difference in OS, though high crossover to crizotinib upon progression on initial chemotherapy compromises such an analysis. Notably, though crizotinib has been generally perceived as having minimal intracranial activity and being insufficient to prevent brain metastases, the recipients of crizotinib demonstrate a significantly lower rate of brain metastases at progression compared to chemotherapy on PROFILE 1014. With greater extracranial as well as intracranial disease control significantly superior with crizotinib, this became the clear standard of care as first line therapy for ALK-positive patients, also providing a clear incentive for seeking to detect an ALK rearrangement. NCCN guidelines came to reflect this with a recommendation to screen patients with non-squamous advanced NSCLC for both activating EGFR mutations and an ALK rearrangement.
More recently, several more potent second generation ALK inhibitors have been studied and proven to have significant efficacy in ALK-positive patients who are either intolerant of or refractory to crizotinib. Over the past several years, patients have benefited from second line or later ceritinib (40,41), alectinib (42), as well as brigatinib (43). These agents all have far greater potency as ALK inhibitors than crizotinib in preclinical studies (44), and all demonstrate good intracranial efficacy in patients with measurable brain metastases (45). These findings have led to second line ALK inhibitors being studied in the first line setting, with the standard of care evolving rapidly. Ceritinib was compared to cisplatin/pemetrexed as first line therapy in the ASCEND-4 trial (46), where ceritinib demonstrated superiority in the primary endpoint of PFS (median 16.6 vs. 8.1 months, HR =0.55, P<0.00001) as well as RR (72.7% vs. 26.7%). Though ceritinib was FDA approved as first line therapy for ALK inhibitor, its challenging toxicity profile and lack of comparison to the most appropriate, current first line standard of care of crizotinib for ALK-positive NSCLC has limited its uptake in this setting. Instead, alectinib has demonstrated remarkably superior efficacy compared to crizotinib as first line therapy in ALK-positive advanced NSCLC in both the Japanese-only phase II J-ALEX trial (47) and the larger, global phase III ALEX trial (48) (see Table 2 for efficacy summary). Notably, the efficacy of alectinib in the first line setting far exceeds those of alectinib in crizotinib-refractory patients. At the present time, alectinib has received a breakthrough designation and priority review for a first line indication for ALK-positive patients (49); on the basis of the available data, it is highly likely to emerge as the clear standard of care as initial systemic therapy in this setting. Notably, newer ALK inhibitors, including brigatinib (50), ensartinib (51), and lorlatinib (52) are also being compared to crizotinib as first-line therapies in head to head prospective trials and may also emerge as compelling alternative first line treatment options.

Full table
With alectinib demonstrating an efficacy far exceeding crizotinib or conventional chemotherapy expectations for both extracranial and intracranial disease control, and potentially newer ALK inhibitors becoming available as comparably or more effective first line therapies for patients with ALK-positive advanced NSCLC, there is a clear incentive to not only identify patients with an ALK rearrangement but to identify them during the initial evaluation. This is the only means by which such patients can avail themselves of the very favorable therapeutic index of alectinib or potentially other agents or combinations that may prove optimal for this patient population in the coming years.
ROS1
Though less well studied than EGFR mutations or ALK rearrangements, ROS1 rearrangements have also emerged as a target for which a targeted therapy has such significant efficacy that it is considered a critical marker to detect as soon as feasible. Such rearrangements are seen in approximately 1–2% of NSCLC tumors, disproportionately more frequently in younger patients and never-smokers with a lung adenocarcinoma (52). In a pivotal series of 50 ROS1-positive patients treated with crizotinib, the demonstrated RR was 82%, with a median duration of response of 17.6 months and median PFS of 19.2 months (53), leading to the FDA approval of crizotinib for this relatively rare indication (54). Though not all ALK inhibitors are also potent inhibitors of ROS1, ceritinib has also been shown to have significant activity (55), including documented activity after acquired resistance to crizotinib (56). At the present time, however, ceritinib is not FDA approved to treat ROS1-positive NSCLC.
Additional studies of this relatively rare molecular subgroup are ongoing at a pace limited by the infrequency of this marker and the prolonged efficacy of crizotinib in patients identified as harboring a ROS1 rearrangement. Though patients with a ROS1 rearrangement represent only a very small minority of NSCLC patients, the remarkable efficacy of crizotinib and potentially ceritinib as well and potentially other targeted therapies still in clinical trials underscores the importance of detecting ROS1 to confer the dramatic and prolonged benefit of ROS1-directed therapy.
Conclusion: what should define the threshold for making detection of a marker in initial workup standard of care?
The array of potentially actionable molecular markers in advanced NSCLC has grown over the past several years, but these targets vary in the extent of data supporting their use, the efficacy of available treatments for them, perhaps modified by their prevalence within the NSCLC population. Though the threshold for a biomarker as mandatory to detect is subject to some interpretation, we might distinguish between biomarkers for which the RR is at least 50% and median PFS at least 8 months and those for which our therapies have lower efficacy. For those patients with an activating EGFR mutation or ALK or ROS1 rearrangement, the efficacy of the associated targeted therapies reliably falls beyond these numbers and far exceeds the expected outcomes for conventional chemotherapy. Moreover, the limited available evidence on the efficacy of immunotherapy for never-smokers and patients with driver mutations, particularly EGFR and ALK, also appears to be far below that seen in other patients (57), providing further value in detecting a therapeutically relevant driver mutation to hone treatment recommendations.
Because these targeted therapies are generally only available to the subgroup in whom the appropriate molecular driver has been detected, it is critical to identify these markers, but this does not equate to a mandate to identify them in the initial workup, before first line therapy has been pursued. It is fair to note that there are not data that clearly demonstrate a significant advantage in patients receiving these targeted therapies as first line vs. subsequent therapy. We can see, however, that in trials of first line targeted therapy vs. chemotherapy in patients with an identified biomarker, the crossover rate to what proves to be optimal first line therapy is inevitably below 100%, sometimes far below that: patients who do not receive the most efficacious therapy first are prone to miss that opportunity. In some cases, first progression is in the CNS and may be accompanied by a prohibitive decline in performance status that could potentially be obviated by initiating treatment with the targeted therapy that often has superior intracranial as well as extracranial efficacy. For some targeted therapies, such as alectinib, the demonstrated efficacy in the first line setting appears to be markedly superior to that of the same therapy later. Overall, the only definite means by which patients can be assured to receive the anticipated substantial benefits of the optimal systemic therapy is by early detection of the relevant molecular driver followed by initiation of the optimal targeted therapy as first line treatment.
While other biomarkers that are emerging as candidates for being considered as an arguable standard of care to detect in advanced NSCLC, they should be measured against the anticipated striking efficacy parameters of EGFR, ALK, and ROS1. By doing so, we can clarify whether the targeted therapy in question represents a consistently highly active therapy with sustained benefit or just one more potential treatment option with a far more limited likelihood of utility, and likely for a far more transient duration. In the coming years, many additional molecular markers will be identified as candidates for targeted therapies. To prioritize and sequence our therapies appropriately, we will need to distinguish between those that should move to the front of the line and others with far more meager data that can rightfully be considered but should not displace therapies with far more established efficacy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author is a consultant/speaker from Ariad, AstraZeneca, Boehringer-Ingelheim, Genentech/Roche, Takeda and received honoraria from Ariad.
References
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Non-Small Cell Lung Cancer, Version 8.2017. Available online: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
- Lynch TJ, Bell DW, Sordella R, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 2004;350:2129-39. [Crossref] [PubMed]
- Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 2004;304:1497-500. [Crossref] [PubMed]
- Food and Drug Adminstration. Center for Drug Evaluation and Research, Oncologic Drugs Advisory Committee Meeting. March 4, 2005. Available online: https://www.fda.gov/ohrms/dockets/ac/05/questions/2005-4095Q1_02_Iressa-Questions.pdf
- Cohen MH, Johnson JR, Chen YF, et al. FDA drug approval summary: erlotinib (Tarceva) tablets. Oncologist 2005;10:461-6. [Crossref] [PubMed]
- Shepherd FA, Rodrigues Pereira J, Ciuleanu T, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 2005;353:123-32. [Crossref] [PubMed]
- FDA Approval for Gefitinib. Brand name(s): Iressa®. Available online: https://www.cancer.gov/about-cancer/treatment/drugs/fda-gefitinib
- Thatcher N, Chang A, Parikh P, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet 2005;366:1527-37. [Crossref] [PubMed]
- Kris MG, Natale RB, Herbst RS, et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 2003;290:2149-58. [Crossref] [PubMed]
- Miller VA, Riely GJ, Zakowski MF, et al. Molecular characteristics of bronchioloalveolar carcinoma and adenocarcinoma, bronchioloalveolar carcinoma subtype, predict response to erlotinib. J Clin Oncol 2008;26:1472-8. [Crossref] [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Pao W, Miller V, Zakowski M, et al. EGF receptor gene mutations are common in lung cancers from "never smokers" and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A 2004;101:13306-11. [Crossref] [PubMed]
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [Crossref] [PubMed]
- Gridelli C, Ciardello F, Gallo C, et al. First-line erlotinib followed by second-line cisplatin-gemcitabine chemotherapy in advanced non-small-cell lung cancer: the TORCH randomized trial. J Clin Oncol 2012;30:3002-11. [Crossref] [PubMed]
- Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. [Crossref] [PubMed]
- Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 2010;11:121-8. [Crossref] [PubMed]
- Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 2012;13:239-46. [Crossref] [PubMed]
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. [Crossref] [PubMed]
- Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. [Crossref] [PubMed]
- Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:213-22. [Crossref] [PubMed]
- Takano T, Fukui T, Ohe Y, et al. EGFR mutations predict survival benefit from gefitinib in patients with advanced lung adenocarcinoma: a historical comparison of patients treated before and after gefitinib approval in Japan. J Clin Oncol 2008;26:5589-95. [Crossref] [PubMed]
- Yang JC, Wu YL, Schuler M, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol 2015;16:141-51. [Crossref] [PubMed]
- Park K, Tan EH, O’Byrne K, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol 2016;17:577-89. [Crossref] [PubMed]
- Lohinai Z, Hoda MA, Fabian K, et al. Distinct Epidemiology and Clinical Consequence of Classic Versus Rare EGFR Mutations in Lung Adenocarcinoma. J Thorac Oncol 2015;10:738-46. [Crossref] [PubMed]
- Karachaliou N, Molina-Vila MA, Rosell R. The impact of rare EGFR mutations on the treatment response of patients with non-small cell lung cancer. Expert Rev Respir Med 2015;9:241-4. [Crossref] [PubMed]
- Kazandjian D, Blumenthal GM, Yuan W, et al. FDA Approval of Gefitinib for the Treatment of Patients with Metastatic EGFR Mutation-Positive Non-Small Cell Lung Cancer. Clin Cancer Res 2016;22:1307-12. [Crossref] [PubMed]
- The U.S. FDA. Erlotinib (Tarceva). Available online: https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm525739.htm
- FDA Approval for Afatinib Dimaleate. Brand name(s): Gilotrif™. Available online: https://www.cancer.gov/about-cancer/treatment/drugs/fda-afatinibdimaleate
- Magnuson WJ, Lester-Coll NH, Wu AJ, et al. Management of Brain Metastases in Tyrosine Kinase Inhibitor-Naïve Epidermal Growth Factor Receptor-Mutant Non-Small-Cell Lung Cancer: A Retrospective Multi-Institutional Analysis. J Clin Oncol 2017;35:1070-7. [Crossref] [PubMed]
- AZD9291 Versus Gefitinib or Erlotinib in Patients With Locally Advanced or Metastatic Non-small Cell Lung Cancer (FLAURA). Available online: https://clinicaltrials.gov/ct2/show/NCT02296125
- Tagrisso significantly improves progression-free survival in the Phase III FLAURA trial for lung cancer. Available online: https://www.astrazeneca.com/media-centre/press-releases/2017/tagrisso-significantly-improves-progression-free-survival-in-the-phase-iii-flaura-trial-for-lung-cancer-27072017.html
- The U.S. FDA. Osimertinib (TAGRISSO). Available online: https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm549683.htm
- Piotrowska Z, Sequist LV. Treatment of EGFR-Mutant Lung Cancers After Progression in Patients Receiving First-Line EGFR Tyrosine Kinase Inhibitors: A Review. JAMA Oncol 2016;2:948-54. [Crossref] [PubMed]
- Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007;448:561-6. [Crossref] [PubMed]
- Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol 2009;27:4247-53. [Crossref] [PubMed]
- Cui JJ, Tran-Dubé M, Shen H, et al. Structure based drug design of crizotinib (PF-02341066), a potent and selective dual inhibitor of mesenchymal-epithelial transition factor (c-MET) kinase and anaplastic lymphoma kinase (ALK). J Med Chem 2011;54:6342-63. [Crossref] [PubMed]
- Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010;363:1693-703. [Crossref] [PubMed]
- Kazandjian D, Blumenthal GM, Chen HY, et al. FDA approval summary: crizotinib for the treatment of metastatic non-small cell lung cancer with anaplastic lymphoma kinase rearrangements. Oncologist 2014;19:e5-11. [Crossref] [PubMed]
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. [Crossref] [PubMed]
- Shaw AT, Kim DW, Mehra R, et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N Engl J Med 2014;370:1189-97. [Crossref] [PubMed]
- Kim DW, Mehra R, Tan DS, et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol 2016;17:452-63. [Crossref] [PubMed]
- Shaw AT, Gandhi L, Gadgeel S, et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol 2016;17:234-42. [Crossref] [PubMed]
- Kim DW, Tiseo M, Ahn MJ, et al. Brigatinib in Patients With Crizotinib-Refractory Anaplastic Lymphoma Kinase-Positive Non-Small-Cell Lung Cancer: A Randomized, Multicenter Phase II Trial. J Clin Oncol 2017;35:2490-8. [Crossref] [PubMed]
- Sasaki T, Rodig SJ, Chirieac LR, et al. The biology and treatment of EML4-ALK non-small cell lung cancer. Eur J Cancer 2010;46:1773-80. [Crossref] [PubMed]
- Rusthoven CG, Doebele RC. Management of Brain Metastases in ALK-Positive Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:2814-9. [Crossref] [PubMed]
- Soria JC, Tan DS, Chiari R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet 2017;389:917-29. [Crossref] [PubMed]
- Hida T, Nokihara H, Kondo M, et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet 2017;390:29-39. [Crossref] [PubMed]
- Peters S, Camidge DR, Shaw AT, et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:829-38. [Crossref] [PubMed]
- Pharmaceuticals A. ALTA-1L Study: A Phase 3 Study of Brigatinib Versus Crizotinib in ALK-positive Advanced Non-Small Cell Lung Cancer Patients (ALTA-1L). Available online: https://clinicaltrials.gov/ct2/show/NCT02737501
- Xcovery Holding Company, LLC. eXalt3: Study Comparing X-396 (Ensartinib) to Crizotinib in ALK Positive Non-Small Cell Lung Cancer (NSCLC) Patients. Available online: https://clinicaltrials.gov/ct2/show/NCT02767804
- A Study Of Lorlatinib Versus Crizotinib In First Line Treatment Of Patients With ALK-Positive NSCLC. Available online: https://clinicaltrials.gov/ct2/show/NCT03052608
- Bergethon K, Shaw AT, Ou SH, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol 2012;30:863-70. [Crossref] [PubMed]
- Shaw AT, Ou SH, Bang YJ, et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N Engl J Med 2014;371:1963-71. [Crossref] [PubMed]
- FDA expands use of Xalkori to treat rare form of advanced non-small cell lung cancer. Available online: https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm490329.htm
- Lim SM, Kim HR, Lee JS, et al. Open-Label, Multicenter, Phase II Study of Ceritinib in Patients With Non-Small-Cell Lung Cancer Harboring ROS1 Rearrangement. J Clin Oncol 2017;35:2613-8. [Crossref] [PubMed]
- Subbiah V, Hong DS, Meric-Bernstam F. Clinical activity of ceritinib in ROS1-rearranged non-small cell lung cancer: Bench to bedside report. Proc Natl Acad Sci U S A 2016;113:E1419-20. [Crossref] [PubMed]
- Gainor JF, Shaw AT, Sequist LV, et al. EGFR Mutations and ALK Rearrangements Are Associated with Low Response Rates to PD-1 Pathway Blockade in Non-Small Cell Lung Cancer: A Retrospective Analysis. Clin Cancer Res 2016;22:4585-93. [Crossref] [PubMed]


