Economic evaluation of different suture closure methods: barbed versus traditional interrupted sutures
Introduction
Along with the success of total knee arthroplasty (TKA) comes the economic burden associated with these surgeries. With the onset of newer policies and the dynamic state of the healthcare system, hospitals are having a higher degree of financial accountability. Healthcare systems are also receiving increasing pressures from payers, such as the Centers for Medicare and Medicaid (CMS) to reduce the costs associated with procedures, and the implementation of the Affordable Care Act aims to address high costs through pay for performance programs. Thus, multiple areas of the TKA surgery are under scrutiny, including surgical times, material costs, and the cost of associated complications and readmissions (1). There are a multitude of variables that affect these factors, one of which is wound closure. Closure can often be a time consuming and considerable part of the surgery, and reducing this time has been targeted as a method of cost management. Suture type has been determined to be a factor that may influence closure time and thus costs, as well as having effect on direct material costs (2).
Traditionally, wound closure for TKA involves using interrupted sutures for multiple layers of fascia, subcutaneous, and cutaneous tissue. Disadvantages associated with this method were thought to be the increased operative time, local tissue ischemia, and increased material use with subsequent costs. Barbed sutures, and those that are bidirectional in nature, were recently introduced to allow for simultaneous closure from the wound center (3). Studies have demonstrated that the use of barbed knotless sutures allows for a faster and more efficient closure with less material used, while providing a watertight arthrotomy closure (2).
However, whether these purported advantages translate to lower overall costs has been questioned. The purpose of this literature review was to compare: (I) the costs of using barbed to conventional interrupted sutures; (II) the additional costs of differences in complications, if any; (III) to extrapolate cost savings on hospital and national level; and (IV) to discuss the role of these findings on hospital savings and the effects on bundled payments.
Methods
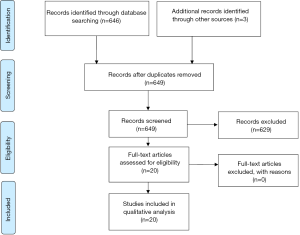
A thorough literature search was conducted using three electronic databases: PubMed, EBSCO Host, and SCOPUS. All available studies between 1989 and 2017 were evaluated. Searches were performed using the following terms: arthroplasty* (title), knee (title), post-operative outcome (title), complication (title), wound closure (title), suture (title), deep (title), superficial (title), barbed suture (title), cost (title); CMS (title); closure time (title), bundled payments (title) and closure technique (title), and ‘knee’, and ‘suture’. Other search terms included: ‘knee arthroplasty’, ‘knee replacement’, and ‘wound closure review’. This yielded 646 reports. We included reports on costs associated with barbed and traditional interrupted sutures in TKA. Through a title and abstract review, we determined the relevant manuscripts, which were subsequently recovered in full and studied. A total of 17 reports satisfied the criteria. We also searched reference lists of retrieved reports and articles and added another 3 reports. Preference was given to meta-analyses, randomized-controlled trials, and data from national registries. However, all studies thought to be relevant to our topic were included. A total of 20 studies were included in this review (Figure 1). We primarily used 9 TKA reports, but when necessary, we referred to reports for other orthopaedic fields as well as non-orthopaedic specialties, to corroborate out findings.
Cost comparison between barbed and interrupted sutures
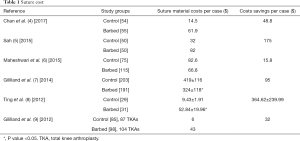
Many studies have compared costs between barbed and standard interrupted sutures, and many have shown that shorter operative times in the barbed cohorts correlated with lower costs (Table 1). Ting et al. (8) conducted a prospective, randomized trial comparing outcomes in 65 TKA or THA patients who underwent primary closure with barbed suture or a combination of interrupted sutures (traditional cohort). For individual suture cost, it was found that the cost per stitch for monofilament absorbable sutures ranged between 1.75 to 1.83 USD, and the cost per stitch for barbed sutures was 19.96 USD. In the TKAs, the mean cost per patient for barbed sutures was significantly higher than for traditional interrupted (53 vs. 9 USD; P=0.002). However, when the authors factored in the mean savings in closure time associated with the barbed sutures (+4 minutes), the authors determined that the cost per unit of operative time was actually lower in the barbed cohort. The mean savings in dollars per patients closed using the barbed suture was 364 USD for TKAs (8).
Full table
Chan et al. (4) compared the costs of barbed versus traditional sutures in 109 primary TKAs. Suture material cost was calculated by multiplying the cost of each suture and the number of sutures used per TKA. The cost of barbed suture material is 47.4 USD more than the traditional suture for each TKA. They noted that traditional sutures led to slower arthrotomy closure time (491 vs. 325 seconds), thus leading to higher savings in the barbed cohort. Considering both suture material and operation cost, barbed suture on average saved USD 48.8 per TKA (4). In addition, Zhang et al. (10) conducted a systematic review and meta-analysis of 9 studies comparing the use of knotless barbed sutures to standard interrupted sutures. Based on an analysis of the pooled data, it was noted that the barbed suture was associated with USD 290.72 lower costs than the standard knotted sutures, taking into account material cost and closure time (10).
Sah (5) compared barbed to traditional interrupted sutures in 50 TKA patients. The author noted that the barbed suture led to a mean faster closure time of 4.7 minutes (P<0.001). Although the material cost was higher in the barbed suture cohort compared to the interrupted group (82 vs. 32 USD), the barbed sutures still led to greater savings (+175 USD per case, range 100 to 250 USD), which were attributed to faster closure time. The author noted no significant differences in post-operative Knee Society Scores (93 vs. 93 points; P=0.6) or range of motion (127 vs. 126 degrees; P=0.4) between the groups, thus demonstrating that cost savings with barbed sutures do not come at cost to the patient outcomes (5).
Studies have also demonstrated lower costs with barbed sutures despite no differences in closure time when compared to standard interrupted sutures. Maheshwari et al. evaluated the cost-effectiveness of barbed versus standard sutures in 333 TKAs and noted that there were no significant differences in closure time between the cohorts (31 vs. 30 minutes; P>0.05) but barbed sutures had a lower overall material cost (66.78 vs. 82.59 USD) (6). The lower overall material cost in barbed suture cohort might be attributed to lower number of individual sutures needed to close a layer of the wound. A single barbed suture might suffice for an area that needs 2 or more standard sutures.
Conversely, studies have demonstrated no differences in cost. In a retrospective study, Gililland et al. (9) compared closure time, costs, and associated complications between barbed sutures and an interrupted suture technique in 191 primary TKAs. As with most of the above studies, mean closure time was faster in the barbed cohort compared to the standard interrupted group (20 vs. 22 minutes; P<0.009). However, they noted that the material cost of the barbed sutures was higher (43 versus 6 USD). As a result, there was no difference in total closure cost between the groups (595 vs. 627 USD; P=0.26). Furthermore, the rate and type of perioperative complications between the groups was similar, thus not affecting overall cost (9). However, in a prospective study, Gililland et al. (7) found that final costs per case reported, which included operative room consumables and suture materials, were significantly lower in the barbed suture group (barbed vs. traditional: 324±118 vs. 419±116 USD; P<0.001).
The majority of the above studies demonstrate that the main factors affecting the differences in overall cost between barbed and standard interrupted suture are material cost and closure time. Material cost of an individual barbed suture is certainly higher than that of a conventional interrupted suture. However, in many cases, a single barbed suture may be sufficient for closure of a single wound layer, while multiple conventional suture is required for interrupted closure. Therefore, despite the higher material cost of barbed sutures, they may lead to an overall lower, or at least equivalent, cost burden due to shorter operative times and smaller number of individual sutures needed for closure.
Costs associated with complications
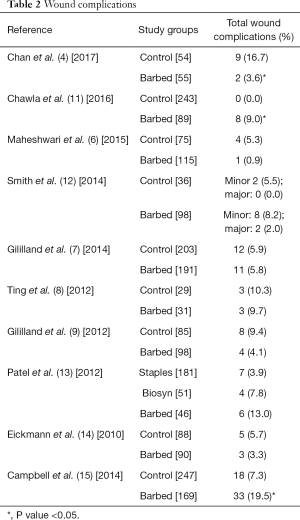
The costs associated with post-operative complications and readmissions can be considerable. Areas that are highly targeted for cost reduction include post-operative surgical site infections, hospital length of stay, and subsequent risk of readmission. Often, wound complications after surgery are associated with closure method and include wound dehiscence, stitch abscess, and drainage, among others, which may subsequently affect length of stay and readmissions (Table 2). In El Bitar et al. (16) study using the Nationwide Inpatient Sample (NIS), both infection and mechanical wound complications were among the top factors associated with increased length of stay in primary TKA (odds ratio, 10.25 and 10.37) (16). Furthermore, Sibia et al. (17) demonstrated that hospital costs for emergency department visits or readmissions exceeded 150,000 USD, and the largest collective costs were incurred with treatments for wound infections (17).
Full table
However, there is limited evidence on the effect of wound closure type on post-operative length of stay. Eggers et al. (18) conducted a prospective, randomized study comparing adhesives, staples, and Monocryl sutures for cutaneous closure in 90 TKAs. The cost was highest for the suture cohort, followed by the adhesive cohorts, then the staples (75 vs. 70, 62, and 57 USD, respectively). The authors factored in labor costs and staple removal cost. However, the staple cohort had a 33% higher length of stay, and when the associated medical expenses where included, it was found that the staple group had an 18% increase in cost when compared to the suture cohort. Therefore, it is important to note that costs associated with closure are not only attributed to the material or closure time, but are also affected by differences in post-operative complications and length of hospital stay (18).
When evaluating complications specifically associated with barbed versus traditional sutures, it is theorized that knots may place uneven pressure on tissue causing ischemia, or they may cause local tissue inflammation and serve as a nidus for infection. In addition, it is thought that knotless barbed sutures provide a more uniform tension on the tissue and therefore reduce the risk of local tissue ischemia (10).
Borzio et al. (1) conducted a systematic review and meta-analysis comparing four level one studies that evaluated costs associated with different suture types in THA and TKA. Factors included in costs were complication rates, cost of suture material, and closure time. It was found that major and minor complication rates between barbed suture and conventional suture cohorts were nearly the same (95% CI: 0.31–0.54; P=0.95), thus not contributing to cost differences between the groups. Closure time was significantly faster in the barbed cohorts, which ultimately led to greater costs savings in barbed closure cohorts compared to standard suture in TKA patients (58 to 365 USD) (1). Similarly, Maheshwari et al. (6) compared barbed to standard sutures in 333 TKAs and noted similar complication rates, but the barbed cohort had a lower overall cost (6).
There are no TKA studies evaluating the effect of wound complications such as infection or dehiscence and subsequent readmission and re-operation on costs between barbed and conventional sutures. Several studies in other specialties demonstrate decreased infection and dehiscence rates in closure with barbed, when compared to conventional sutures. Ahmed et al. (19) performed a retrospective study of 715 wound closures (273 barbed, 442 conventional) after power-injectable dual-lumen chest port placement and demonstrated lower dehiscence (0 vs. 1.6%; P=0.04) and infection (5.1% vs. 9.5%; P=0.03) rates in barbed vs. conventional closure. If the use of barbed sutures decreases the rate of revisions for infection and readmission in TKA patients, tremendous cost savings could be achieved. Kapadia et al. (20) performed retrospective review of prospectively collected single hospital infection database and identified 21 patients who underwent revision TKA for infection and matched them to 21 patients who had an uncomplicated primary TKA. The annual mean healthcare cost for infected TKA was significantly higher than for non-infected TKA (116,383 vs. 28,249 USD; P<0.0001), which amounted to 88,134 USD difference. According to a NIS database study by Bozic et al. (21), there were 73,878 revision total knee arthroplasties due to infection performed in a 5-year period between 2005 and 2010. If the infection rate in TKA was reduced by 44%, as in a study of chest port placement by Ahmed et al., there would be 32,506 less cases of revision TKA for infection over a 5-year period, which would account to almost 3 billion USD in savings.
Hospital and national level extrapolation
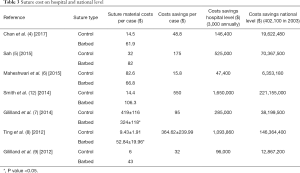
The cost savings achieved by using barbed sutures for the individual procedures may not amount to marked cost savings. However, when these savings are extrapolated to a hospital and, more importantly, to a national level, they constitute a considerable amount of healthcare budget (Table 3). We extrapolated these costs to a single center (3,000 cases annually) and to national level (402,100 cases in 2003) (22). The cost savings on the hospital level amounted to a mean of 549,094 USD (range, 47,400 to 1,650,000 USD). The cost savings on the national level amounted to a mean of 73,561,323 USD (range, 6,353,180 to 221,155,000 USD).
Full table
Does this have a role in bundled payments?
Many of these studies that have demonstrated faster closure time show differences of a few minutes. Although these have been represented to be statistically significant, it is questionable whether such a small margin of time is clinically relevant. Thus, the purported time saved may not actually translate into real healthcare dollars. This is particularly true when many hospitals bill on an hourly rate, and thus it can be argued that if the time saved does not exceed an hour, then these minute reductions may do nothing to affect overall cost (23).
The bundled payment for care improvement (BPCI) initiative has been developed by the Centers for Medicare and Medicaid Services to promote efficient and low-cost care. Per Miletic et al. (24), 1% of TKA patients had an unplanned hospitalization for a surgical site infection within the year, and 30% of these were subsequently re-hospitalized, each associated with a mean cost of 20,000 USD (24). In order to reduce the incidence of unplanned readmissions, surgeons are targeting the causes of surgical infections post-operatively. Therefore, determining the complications and incidence of infections associated with different wound closure techniques is crucial in reducing the risk of penalty in the bundled payment scheme. Based on the above studies, complication rates have been shown to be similar so far, but there is limited study on the costs associated with these in TKA patients. There must be more focus on the effect of different suture types on readmissions and revisions, particularly as this plays a considerable role in reimbursements.
A further limitation in these cost analyses is the difficulty in comparing outcomes between institutions. Standard protocols vary between hospitals. The number of sutures used and speed vary between surgeons, let alone among different practices. These are among the many variables that influence the purported cost savings and prevent consistent and reliable comparisons, which may ultimately be why no true consensus has yet been reached on this topic.
Although the majority of the literature has demonstrated no differences in actual complication rates, there are no studies to our knowledge that systematically evaluate whether the complications associated with these suture types are linked to an increased need for readmissions. However so far, barbed sutures may prove to be a promising modification to improve the TKA experience, but further studies are needed to directly correlate the direct costs of specific complications and associated readmissions in TKA patients.
Conclusions
There is a considerable economic burden associated with TKAs, and hospitals are under increasing pressures to drive down cost. Areas of interest include reducing operative time, material cost, and incidence of post-operative complications. The use of barbed sutures has been shown to reduce operative time and thus total cost when compared to interrupted sutures, while demonstrating similar post-operative complication rates. However, based on the available literature, there is no evidence on the direct costs of complications associated with different suture material, nor are there studies on the effect of these complications on length of stay and readmissions in TKA patients. Due to the lack of these studies in TKA patients, we have demonstrated potential costs savings associated with the use of barbed sutures in TKA patients based on the lower infection rates in other specialties. Reduction in TKA infection and subsequent revision rates could amount to almost 3 billion dollars in cost savings. In order to determine the true effect of the cost reductions associated with shorter closure time and decrease in infection burden when using barbed sutures, further prospective studies are needed to answer these questions. Specifically, studies that compare revision rates due to infection between patients who receive barbed versus conventional sutures for TKA, as well as their correlation with costs need to be performed.
Acknowledgements
The preparation of this manuscript was partially funded by an educational grant from Ethicon Inc.
Footnote
Conflicts of Interest: Dr. Mont is a paid consultant for Ethicon Inc. and receives research support from Ethicon Inc. Dr. Elmallah is a paid consultant for Ethicon Inc. The other authors have no conflicts of interest to declare.
References
- Borzio RW, Pivec R, Kapadia BH, et al. Barbed sutures in total hip and knee arthroplasty: what is the evidence? A meta-analysis. Int Orthop 2016;40:225-31. [Crossref] [PubMed]
- Mansour A, Ballard R, Garg S, et al. The use of barbed sutures during scoliosis fusion wound closure: a quality improvement analysis. J Pediatr Orthop 2013;33:786-90. [Crossref] [PubMed]
- Levine BR, Ting N, Della Valle CJ. Use of a Barbed Suture in the Closure of Hip and Knee Arthroplasty Wounds. Orthopedics 2011;34:e473-5. [PubMed]
- Chan VW, Chan PK, Chiu KY, et al. Does Barbed Suture Lower Cost and Improve Outcome in Total Knee Arthroplasty? A Randomized Controlled Trial. J Arthroplasty 2017;32:1474-7. [Crossref] [PubMed]
- Sah AP. Is There an Advantage to Knotless Barbed Suture in TKA Wound Closure? A Randomized Trial in Simultaneous Bilateral TKAs. Clin Orthop Relat Res 2015;473:2019-27. [Crossref] [PubMed]
- Maheshwari AV, Naziri Q, Wong A, et al. Barbed Sutures in Total Knee Arthroplasty: Are These Safe, Efficacious, and Cost-Effective? J Knee Surg 2015;28:151-6. [PubMed]
- Gililland JM, Anderson LA, Barney JK, et al. Barbed versus standard sutures for closure in total knee arthroplasty: a multicenter prospective randomized trial. J Arthroplasty 2014;29:135-8. [Crossref] [PubMed]
- Ting NT, Moric MM, Della Valle CJ, et al. Use of knotless suture for closure of total hip and knee arthroplasties: a prospective, randomized clinical trial. J Arthroplasty 2012;27:1783-8. [Crossref] [PubMed]
- Gililland JM, Anderson LA, Sun G, et al. Perioperative closure-related complication rates and cost analysis of barbed suture for closure in TKA. Clin Orthop Relat Res 2012;470:125-9. [Crossref] [PubMed]
- Zhang W, Xue D, Yin H, et al. Barbed versus traditional sutures for wound closure in knee arthroplasty: a systematic review and meta-analysis. Sci Rep 2016;6:19764. [Crossref] [PubMed]
- Chawla H, van der List JP, Fein NB, et al. Barbed Suture Is Associated With Increased Risk of Wound Infection After Unicompartmental Knee Arthroplasty. J Arthroplasty 2016;31:1561-7. [Crossref] [PubMed]
- Smith EL, DiSegna ST, Shukla PY, et al. Barbed versus traditional sutures: closure time, cost, and wound related outcomes in total joint arthroplasty. J Arthroplasty 2014;29:283-7. [Crossref] [PubMed]
- Patel RM, Cayo M, Patel A, et al. Wound complications in joint arthroplasty: comparing traditional and modern methods of skin closure. Orthopedics 2012;35:e641-6. [Crossref] [PubMed]
- Eickmann T, Quane E. Total knee arthroplasty closure with barbed sutures. J Knee Surg 2010;23:163-7. [Crossref] [PubMed]
- Campbell AL, Patrick DA, Liabaud B, et al. Superficial wound closure complications with barbed sutures following knee arthroplasty. J Arthroplasty 2014;29:966-9. [Crossref] [PubMed]
- El Bitar YF, Illingworth KD, Scaife SL, et al. Hospital Length of Stay following Primary Total Knee Arthroplasty: Data from the Nationwide Inpatient Sample Database. J Arthroplasty 2015;30:1710-5. [Crossref] [PubMed]
- Sibia US, Mandelblatt AE, Callanan MA, et al. Incidence, Risk Factors, and Costs for Hospital Returns After Total Joint Arthroplasties. J Arthroplasty 2017;32:381-5. [Crossref] [PubMed]
- Eggers MD, Fang L, Lionberger DR. A comparison of wound closure techniques for total knee arthroplasty. J Arthroplasty 2011;26:1251-8.e1. [Crossref] [PubMed]
- Ahmed O, Jilani D, Funaki B, et al. Comparison of Barbed versus Conventional Sutures for Wound Closure of Radiologically Implanted Chest Ports. J Vasc Interv Radiol 2014;25:1433-8. [Crossref] [PubMed]
- Kapadia BH, McElroy MJ, Issa K, et al. The Economic Impact of Periprosthetic Infections Following Total Knee Arthroplasty at a Specialized Tertiary-Care Center. J Arthroplasty 2014;29:929-32. [Crossref] [PubMed]
- Bozic KJ, Kamath AF, Ong K, et al. Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA. Clin Orthop Relat Res 2015;473:2131-8. [Crossref] [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Levine BR. CORR Insights®: Is There an Advantage to Knotless Barbed Suture in TKA Wound Closure? A Randomized Trial in Simultaneous Bilateral TKAs. Clin Orthop Relat Res 2015;473:2028-30. [Crossref] [PubMed]
- Miletic KG, Taylor TN, Martin ET, et al. Readmissions after Diagnosis of Surgical Site Infection Following Knee and Hip Arthroplasty. Infect Control Hosp Epidemiol 2014;35:152-7. [Crossref] [PubMed]