Impact of diverticular inflammation and complication assessment classification on the burden of medical therapies in preventing diverticular disease complications in Italy
Introduction
Colonic diverticulosis is an age-related disease that affects approximately 25% of the westernized world (1). It is characterized by asymptomatic sac-like protrusions (called “diverticula”) in the colonic wall that form when the mucosa herniates at weak points in the muscularis propria; these weak points occur where blood vessels enter to supply the colonic wall (1). Although most patients with pathologic evidence of colonic diverticula are asymptomatic, about 20% of patients develop symptoms such as abdominal discomfort and altered bowel habits: these patients are said to have symptomatic diverticular disease (DD) (1).
Gastrointestinal, liver, and pancreatic diseases are highly prevalent, costly, and lead to substantial health care utilization. In United States many of these diseases also affect patients’ quality of life and productivity (2), so that the National Institutes of Health plans to devote an estimated $1.6 billion to gastrointestinal research and another $619 million to liver disease research in 2015 (3).
DD and its complications represent a burden for the health systems all over the world (4). For example, recent data, obtained from the 2010 National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey from the United States, report that DD is the eighth most frequent outpatient gastrointestinal, with an aggregate cost of 2.2 billion of USD (5).
In Italy, there are no specific data about the global burden on DD. In particular, we don’t have data about the costs for visits, recovery, surgery and related complications, time of work, for patients with DD. Costs are unknown also for outpatient’s treatments in order to prevent DD complications, in particular in preventing acute diverticulitis occurrence/recurrence. Despite low occurrence of complications, mainly as acute diverticulitis occurrence (6) or recurrence (7), in Italy several scheduled approaches on this topic have been developed (1). However, these approaches may be quite expensive (8), so that selective criteria to identify which and how DD patients should be treated is mandatory. The recent Diverticular Inflammation and Complication Assessment (DICA) endoscopic classification may be a useful tool (9). We recently found that scheduled treatment of DICA 1 and DICA 3 patients did not significantly affect the occurrence of acute diverticulitis occurrence/recurrence and the prevention of surgery occurrence (10). In particular, DICA 1 patients are always at lower risk and DICA 3 patients are always at higher risk of DD complication irrespective of scheduled treatment in order to prevent complications occurrence (10). Only DICA 2 patients seemed to have a significant benefit from a scheduled treatment during the follow-up, and only two types of treatments seemed to be effective (10).
The aim of the present study was to assess the economic evaluation of using DICA classification on the burden of medical therapies prescribed in Italy in order to prevent DD complications.
Methods
As stated, there are no data neither on diverticulosis occurrence neither on DD occurrence nor on DD complications occurrence in Italy. Thus, we estimated the Italian diverticulosis prevalence according to data population at the beginning of 2015, provided by Italian Institute of Statistic (ISTAT) (11), and considering that the prevalence of diverticulosis is estimated to be about 20% of general population (12).
As stated, several treatment are currently prescribed in the Italian people having diverticulosis in order to prevent acute diverticulitis occurrence/recurrence and surgery occurrence (13,14). In particular, four main treatments are currently prescribed.
- Cyclic treatment with rifaximin 800 mg/day for 7–10 days/month;
- Mesalazine 1.6 g/day for 10 days/month or as daily treatment;
- Association rifaximin 800 mg/day plus mesalazine 1.6 g/day for 7 days/month;
- Probiotics, for 10–15 days/month.
Costs of those treatments were analyzed according to official costs reported on the website of the Italian National Agency for Drugs (AIFA) (15), and were reported in euros (€).
- Rifaximin: €19.404 (if prescribed for 7 days/month) – €27.72 (if prescribed for 10 days/month);
- Mesalazine: €8.40 (if prescribed for 10 days/month) – €25.20 (if prescribed daily);
- Rifaximin plus mesalazine association: €19.404 + €5.88 (overall €25.284).
We also analyzed the costs per month of the probiotic treatment with Lactobacillus casei DG, which was the most prescribed probiotic in the DICA study (voce), which was: €5.995 (for 10 days/month).
DICA classification is an endoscopic classification recently developed in order to have homogeneous classification of patients having diverticula detected during colonoscopy. It subdivides patients as having three increasing score of severity: DICA 1, DICA 2, and DICA 3 (9). We found that this classification was able to predict the outcome of the disease according to DICA score severity in term of acute diverticulitis occurrence/recurrence and in term of surgery occurrence (10). Moreover, the same study found that only DICA 2 patients might benefit from a scheduled therapy during the follow-up in term of acute diverticulitis occurrence/recurrence and in term of surgery occurrence (10).
Results
Considering that at 01 January 2015, the Italian population was 60,795,612 and that about 20% this people was estimated having diverticulosis, we estimated that over 8 million of Italian people >60 years had diverticulosis.
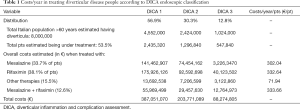
In the retrospective DICA study, we found that 56.9% of the enrolled people were on DICA 1, 30.3% on DICA 2 and 12.8% on DICA 3. If we apply these percentages to population estimated to have diverticulosis, we estimated that 4,552,000 people might be classified as DICA 1; 2,424,000 as DICA 2; and 1,024,000 as DICA 3.
In the retrospective DICA study, we found that 56.9% of the enrolled people had a scheduled treatment during the follow-up in order to prevent DD complication (acute diverticulitis occurrence/recurrence). If we apply these percentages to the population estimated to have diverticulosis, we estimated that 2,435,320 DICA 1; 1,296,840 DICA 2; and 547,840 DICA 3 patients may receive a scheduled treatment during the follow-up in order to prevent DD complication.
Analyzing the treatments reported during the DICA retrospective study, three main treatments were prescribed.
- Cyclic treatment with rifaximin 800 mg/day for 7 or 10 days/month. It was prescribed in 38.1% of the overall population;
- Mesalazine 1.6 g/day for 10 days/month or as daily treatment. It was prescribed in 33.7% of the overall population;
- Association rifaximin 800 mg/day plus mesalazine 1.6 g/day for 7 days/month. It was prescribed in 12.6% of the overall population.
Several other treatments, ranging from fibers to spasmolytics, were prescribed in 15.5% of the overall population. The vast majority of them were treated with probiotics for 10 or 15 days/month. In this way, we analyzed the cost of treatment with capsules containing 16 billion of a specific strain, Lactobacillus casei DG (Enterolactis plus®, Sofar SpA, Trezzano Rosa, Italy), which was the most frequently prescribed probiotic strain in the enrolled patients.
Calculating per patient costs during one year of treatment, we had the following costs:
- Rifaximin: €332.64 (if prescribed for 10 days/month);
- Mesalazine: €302.04 (if prescribed daily);
- Rifaximin plus mesalazine association: €232.86 + €100.8 (overall €333.66);
- Lactobacillus casei DG: €71.94 (for 10 days/month).
Calculating costs per year according to DICA score, we can estimate an overall cost of €387,051,070 for DICA 1; 203,771,089 for DICA 2; and 88,274,805 for DICA 3 patients. Taking into account that DICA 1 patients are always at very low risk of complications, and that DICA 3 patients are always at very high risk of complications despite scheduled therapy, we can conclude that scheduled therapy in term of acute diverticulitis occurrence/recurrence and in term of surgery occurrence prevention seems to be ineffective in DICA 1 and DICA 3 patients. Thus, we can estimated that the overall costs for DICA 1 and DICA 3 patients, namely a total of €475,325,875 million could be inappropriate in managing DD patients in term of acute diverticulitis occurrence/recurrence and in term of surgery occurrence prevention (Table 1).
Full table
Discussion
DD is still a neglected disease, but its epidemiological impact is substantial. Delvaux (16) in 2003 reported an estimation of burden of DD on health care systems in the European Union, at that time consisted of 15 countries with an overall population of >376 million of inhabitants. According to the assumptions obtained from available epidemiological data, Delvaux concluded that about one-third of European population (>100 million people) had diverticula with an annual rate of hospital admissions of 209 per 100,000, corresponding to almost 800,000 hospital admissions (16) In the same paper, the mortality rate for patients admitted for DD was 3%, corresponding to 23,605 deaths/year (16). Similar results come from outside European Union. Data obtained from the Scottish Morbidity Records confirmed that DD was an increasing burden on health service resources, particularly in younger age groups (17). More recently, inpatient gastrointestinal, liver and pancreatic discharge diagnoses from the 2012 Nationwide Inpatients Sample in United Stated reported that diverticulitis without hemorrhage admissions were >216,000 (5). In the same report, diverticular hemorrhage, included in gastrointestinal hemorrhage diagnosis, that was the most frequent diagnosis of admission with >500,000 cases in 2012, had an adjunctive burden of admissions and costs (5). When all the causes of death for gastrointestinal, liver and pancreatic diseases in the United States were considered, the rank of DD in 2012 was 16th with a crude rate of 0.9 per 100,000 patients (5). In term of burden for National Health Systems, authors found an increase of 21% when compared with 2003 data, with an aggregate cost of 2.2 billion of US dollars (5).
The vast majority of these data belonging to hospitalized patients. No clear data about DD burden for Italian National Health System are available, neither for hospitalized patients nor for outpatients. A very preliminary report estimated as €63.5 million/year the burden of hospitalized DD in Italy (18), while an analysis performed in 2010 on outpatient treatment with rifaximin estimated as €245.28/year per patient, overall €301,587,212 million, the hypothetical burden of this treatment (8).
This study focused on the burden of costs in outpatients in order to prevent acute diverticulitis occurrence/recurrence and in term of surgery occurrence prevention, because the incidence of DD and its complications appears to be increasing and the number of patients with DD can be expected to increase in coming years in accordance with current trends, as the population continues to age. For example, United States overall annual age-adjusted admissions for acute diverticulitis increased at a rate of 26% from 1998 to 2005 and rates of admission increased significantly in both younger and older people. Moreover, elective operations for diverticulitis rose up to 29% in the same period, especially in younger people (73% in rates of surgery for those individuals) (19). We have recently found DICA endoscopic classification as predictor of the outcome of DD in term of prevention of acute diverticulitis occurrence/recurrence and in term of surgery occurrence prevention: DICA 1 patients were always at very low risk of complications, and DICA 3 patients were always at very high risk of complications, despite scheduled therapy (10). Scheduled treatments in order to prevent acute diverticulitis occurrence/recurrence and surgery occurrence seem to be appropriated only in DICA 2 patients, and the mesalazine-based and the association mesalazine/rifaximin are the only treatments significantly effective (10).
This study found that DICA classification might be useful and appropriate in term of cost saving in DD management. We estimated that >€475 million could be inappropriate in managing outpatient DD in term of acute diverticulitis occurrence/recurrence and in term of surgery occurrence prevention when prescribed in DICA 1 and DICA 3 patients. This means that the DICA classification, when correctly used in real life, could significantly reduce inappropriateness of outpatient management, saving costs.
This study has three main limits. The first is that no data are currently available about burden of DD in Italy, neither about hospitalization neither about pharmaceutical costs in preventing disease complication. As consequence, this limited the impact of the pharmacoeconomic analysis of this study. The second is that this study focused its attention only on the two main outcomes in DD, namely cost/effectiveness of acute diverticulitis occurrence/recurrence and surgery occurrence prevention. Although important, these are not the only clinical points in managing DD. We cannot forget that acute diverticulitis occurred in about 4% of the overall patients having diverticulosis (6), and that the vast majority of DD patients experience only symptoms without complications (abdominal pain, bowel habit alteration, etc.) (1). In this way, several treatments tested in controlled trials seem to be effective (10-22). Thus, these treatments may be not cost-effective in preventing acute diverticulitis occurrence/recurrence and in term of surgery prevention, but maybe effective in controlling symptoms (23). The third is that this study analyzed retrospective data. A prospective trial on the predictive value of DICA classification is currently ongoing. A new economic analysis about the impact of this classification on the burden of DD is therefore warranted.
In conclusion, DICA endoscopic classification may be useful, helping to select both DD people who actually need treatments and cost/effective treatments in terms of prevention of acute diverticulitis occurrence/recurrence and surgery occurrence.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management of diverticulosis and diverticular disease of the colon. Aliment Pharmacol Ther 2015;42:664-84. [Crossref] [PubMed]
- Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143:1179-87.e1-3.
- Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). Available online: http://report.nih.gov/categorical_spending.aspx
- Papa A, Papa V. The Economic Burden of Diverticular Disease. J Clin Gastroenterol 2016;50 Suppl 1:S2-3. [Crossref] [PubMed]
- Peery AF, Crockett SD, Barritt AS, et al. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology 2015;149:1731-41.e3. [Crossref] [PubMed]
- Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 2013;11:1609-13. [Crossref] [PubMed]
- Trenti L, Kreisler E, Galvez A, et al. Long-term evolution of acute colonic diverticulitis after successful medical treatment. World J Surg 2015;39:266-74. [Crossref] [PubMed]
- Zullo A, Hassan C, Maconi G, et al. Cyclic antibiotic therapy for diverticular disease: a critical reappraisal. J Gastrointestin Liver Dis 2010;19:295-302. [PubMed]
- Tursi A, Brandimarte G, Di Mario F, et al. Development and validation of an endoscopic classification of diverticular disease of the colon: the DICA classification. Dig Dis 2015;33:68-76. [Crossref] [PubMed]
- Tursi A, Brandimarte G, Di Mario F, et al. Predictive value of the Diverticular Inflammation and Complication Assessment (DICA) endoscopic classification on the outcome of diverticular disease of the colon: An international study. United European Gastroenterol J 2016;4:604-13. [Crossref] [PubMed]
- Indicatori demografici. Available online: https://www.istat.it/it/archivio/180494
- Tursi A, Elisei W, Picchio M, et al. Letter: diverticulosis in inflammatory bowel diseases. Aliment Pharmacol Ther 2014;39:899-900. [Crossref] [PubMed]
- De Bastiani R, Sanna G, Fracasso P, et al. The Management of Patients With Diverticulosis and Diverticular Disease in Primary Care: An Online Survey Among Italian General Pratictioners. J Clin Gastroenterol 2016;50 Suppl 1:S89-92. [Crossref] [PubMed]
- Tursi A, Picchio M, Elisei W, et al. Current Management of Patients With Diverticulosis and Diverticular Disease: A Survey From the 2nd International Symposium on Diverticular Disease. J Clin Gastroenterol 2016;50 Suppl 1:S97-S100. [Crossref] [PubMed]
- Prontuario Farmaceutico Nazionale. Available online: http://www.agenziafarmaco.gov.it/it/content/prontuario-farmaceutico-nazionale
- Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther 2003;18 Suppl 3:71-4. [Crossref] [PubMed]
- Paterson HM, Arnott ID, Nicholls RJ, et al. Diverticular disease in Scotland: 2000-2010. Colorectal Dis 2015;17:329-34. [Crossref] [PubMed]
- Koch M. Gastroenterology towards 2020. Recenti Prog Med 2016;107:255-6. [PubMed]
- Etzioni DA, Mack TM, Beart RW Jr, et al. Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg 2009;249:210-7. [Crossref] [PubMed]
- Bianchi M, Festa V, Moretti A, et al. Meta-analysis: long-term therapy with rifaximin in the management of uncomplicated diverticular disease. Aliment Pharmacol Ther 2011;33:902-10. [Crossref] [PubMed]
- Lahner E, Bellisario C, Hassan C, et al. Probiotics in the Treatment of Diverticular Disease. A Systematic Review. J Gastrointestin Liver Dis 2016;25:79-86. [PubMed]
- Picchio M, Elisei W, Brandimarte G, et al. Mesalazine for the Treatment of Symptomatic Uncomplicated Diverticular Disease of the Colon and for Primary Prevention of Diverticulitis: A Systematic Review of Randomized Clinical Trials. J Clin Gastroenterol 2016;50 Suppl 1:S64-9. [Crossref] [PubMed]
- Tursi A, Picchio M, Elisei W, et al. Management of Patients With Diverticulosis and Diverticular Disease: Consensus Statements From the 2nd International Symposium on Diverticular Disease. J Clin Gastroenterol 2016;50 Suppl 1:S101-7. [Crossref] [PubMed]


