Peroral endoscopic myotomy (POEM) for treating esophageal motility disorders
Introduction
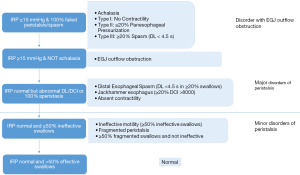
The Chicago Classification v3.0, published in 2015, categorized esophageal motility disorders based on findings in high-resolution manometry. According to a hierarchical approach, it further prioritized the spectrum into (I) “Disorders with esophagogastric junction (EGJ) outflow” including the different types of achalasia and EGJ outflow obstruction; (II) “Major disorders of peristalsis” including distal esophageal spasm, jackhammer esophagus and absent contractility; (III) “Minor disorders of peristalsis” which also appeared in normal controls, including ineffective motility and fragmented peristalsis (Figure 1). Hypertensive contractions were taken out from the classification as it showed no apparent clinical significance. The consensus for the next version of Chicago Classification from different motility societies is eagerly awaited (1). In the previous version of Chicago classification, the term “Spastic Esophageal Disorders” included Type III achalasia, diffuse esophageal spasm and hypercontractile (nutcracker/jackhammer) esophagus (2). They were often studied together as they give rise to similar symptomatology, namely dysphagia, chest pain, regurgitation and heartburn. The overall combined prevalence is approximately 2%. Several pharmacological agents have been tested to decrease the lower esophageal sphincter pressure or reduce hypermotility of the esophageal body. These include calcium channel blockers (e.g., nifedipine), nitrates, sildenafil in some smaller case studies, or even antidepressants. However, the evidence of efficacy is poor, and significant side effects may result, for instance headache, peripheral edema, flushing, and hypotension. More importantly, they do not halt disease progression (3,4).
The incidence of achalasia is around 1 in 100,000 population worldwide, with no gender predilection. It has a bimodal age distribution, with first peak at age 30s to 40s and another after 60s. It is thought to be associated with functional loss of myenteric plexus ganglion cells in the distal esophagus and lower esophageal sphincter. Injection of botulinum toxin only provides temporary effect and it may potentially make subsequent surgery more difficult. Pneumatic dilatation has a successful rate of 62–90%, associated with a small chance of perforation from 0–16% (5). The long-term result of the randomized European Achalasia Trial, which compared pneumatic dilatation with Heller myotomy, was published in 2016. The authors concluded that both pneumatic dilatation with graded distension protocol and laparoscopic Heller myotomy with Dor fundoplication were equally efficient (82% vs. 84%) with at least 5 years of follow up. However, 25% of patients treated with pneumatic dilatation required re-dilatations. In subgroup and risk factor analysis, age less than 40 years, pre-existing daily chest pain, a pre-treatment esophageal width of less than 4 cm and type III achalasia were identified as risk factors for treatment failure or requiring re-dilatation in the pneumatic dilatation group (6).
Endoscopic myotomy was first reported by Pasricha et al. in 2007 in a porcine model (7). In 2010, Inoue et al. published the experience of the first 17 cases of peroral endoscopic myotomy (POEM) patients with modification of the steps of submucosal tunnelling by endoscopic submucosal dissection technique under positive pressure ventilation (8). The publication of a series of 500 patients from his center demonstrated a success rate of 91% in 1–2 years and 88.5% in 3 years (9). Since the introduction of POEM, there have been at least 5000 cases performed worldwide by the end of 2015 and the number is increasing exponentially (10). Yet, there are still a number of controversies on the indications, technical variations, efficacy & complications and application of submucosal tunnelling technique.
Indication
The initial inclusion criteria of the procedure by Inoue et al., was for proven achalasia, with age greater than 18 years, non-sigmoidal esophagus and treatment naïve or uncomplicatedly treated patients (8). Recent publications have shown that the inclusion criteria could be extended to other esophageal motility disorders, to patients of extremes of age, sigmoidal esophagus and re-operated patients.
Spastic esophageal motility disorder
Pharmacological therapy for spastic esophageal disorders, namely Type III achalasia, diffuse esophageal spasm and hypercontractile (nutcracker/jackhammer) esophagus has a relatively low efficacy with unfavourable side effects. The pathophysiology of this group of disease is different with loss of neural inhibition in achalasia and distal esophageal spasm and activation of cholinergic pathway in hypercontractile esophagus. Despite the different mechanisms of disease, POEM provides a logical treatment option equivalent to Heller myotomy with the possibility of extension to the proximal esophagus (11). An international multicentre retrospective study including 73 patients from 11 centers showed that the efficacy in spastic achalasia (96.3%) and distal esophageal spasm (100%) is higher than that of jackhammer esophagus (70%) (12). A more recent meta-analysis included eight observational studies with 179 patients showed a cumulative clinical success rate of 87% (Eckardt score ≤3 and/or improvement of dysphagia by questionnaire). Among the three spastic esophageal motility disorders, Type III achalasia appeared to respond best with 92% success rate, followed by distal esophageal spasm (88%) and hypercontractile esophagus (72%). It concluded that POEM is an effective and safe procedure for spastic esophageal disorders. The mean submucosal tunnel and myotomy length was at 17.2 and 13.5 cm respectively which are significantly longer than that in conventional POEM as concluded in the white paper summary (average myotomy length 8–10 cm) (13,14).
Extreme of age
Achalasia has a bimodal age distribution, with the first peak at age 30s to 40s and another after 60 years. However, it affects patients in all age groups. Inoue et al. reported the youngest patient at 3 years old and the oldest was 89 years old (9). Due to comorbidity and operative risk, many elderly patients would be left untreated or suggested to receive botulinum toxin injection, which is considered suboptimal. POEM is a kind of Natural Orifice Transluminal Endoscopic Surgery (NOTES), which is theoretically less traumatizing than traditional surgical approach. A recently published international multicenter retrospective study of 76 octogenarian patients showed that the adverse event rate was 14.5% while the clinical success rate was 90.8%. There was no 60-day mortality post-POEM. Technical challenge is expected to encounter in geriatric patients as they have (I) higher chance to have previous treatment, (II) longer history of the disease, leading to higher rate of dilated or even sigmoidal esophagus, and (III) they tend to have multiple comorbidities leading to higher operative risk and adverse events (15).
At the other extreme, achalasia is rare in paediatric patients, with an incidence of 0.02–0.11 per 100,000 population. The consequence however is devastating, as it will result in growth retardation both physically and mentally. One cohort study of 27 Chinese paediatrics patients (6–17 years old) reported a 100% successful rate with a mean follow-up of more than 2 years. However, 5 patients (19.2%) had mucosal injury or perforations. The authors attributed the high adverse event rate to technical difficulties, namely narrow lumen and fragile mucosa (16). Another study in India with 15 paediatric patients again reported 100% clinical response rate and 6.7% mucosal injury rate (17). From technical point of view, the endoscopist should consider using a smaller size endoscope and blunt dissection for submucosal tunnelling.
Sigmoidal esophagus and patients with prior treatment
Sigmoidal esophagus is graded into S1 (where there is only one lumen seen in CT scan) and S2 (when tortuosity and U-turn leading to two lumens in CT scan). Inoue et al. initially only included non-sigmoidal achalasia and later extended the indication to more advanced cases. His first 500 cases included 48 S1 and 29 S2 patients. The pooled success rate was 91% in 1–2 years and 88.5% in 3 years (8,9). Hu et al. published a cohort of 32 sigmoidal achalasia patients (29 S1, 3 S2), clinical treatment success rate was 96.8%. The mucosal injury rate was fairly high at 37.5%. Some technical advices suggested by the author included: (I) to design a straight path for submucosal tunnelling, e.g., posterior wall of esophagus along the spine; (II) to navigate in the tunnel perpendicular to circular muscle layer; (III) to expect a higher mucosal perforation rate because of fibrosis and limited space within the tunnel; (IV) POEM for sigmoidal esophagus should be performed in expert centers (18).
The European Achalasia Trial concluded that both pneumatic dilatation with graded distension protocol and laparoscopic Heller myotomy with Dor fundoplication were equally efficient (82% vs. 84%) with at least 5 years of follow up (6). However, 10–20% of patients suffered from persistent or recurrent of symptoms. This leads to the discussion on whether “salvage/rescue POEM” is possible and advisable. The POEM white paper summary published in 2014, collecting data from the International POEM Survey (IPOEMS) and 16 expert centers, showed that 43% of the operated patients had prior failed treatment (including botulinum injections). The consensus suggested that prior treatment would result in significant fibrosis in the submucosal layer that might result in a slower and more challenging dissection and increase procedure time. Despite the technical difficulty, the efficacy remained excellent (14,19,20). A recent retrospective cohort study in 13 tertiary centers included data of 180 patients (90 with prior Heller myotomy and 90 matched patients with no prior Heller myotomy). The technical success rate (98% vs. 100%) and procedure time were comparable. The clinical response was significantly lower in prior myotomy group (81%) vs. no prior myotomy group (94%). The adverse effect rate was not significantly different between the two groups (8% in prior myotomy group vs. 13% in no prior myotomy group). The authors concluded that although the clinical efficacy rate was lower, it could still be advised as the preferred therapeutic option due to its minimal invasiveness and relative safety (21).
Technical variation
The initial procedure involves creation of a submucosal tunnel beginning at 13 cm proximal to the gastroesophageal junction (GEJ) and extending 3 cm into the proximal stomach. Anterior myotomy starts at 7 cm above GEJ and extends 2 cm distally. Completion of procedure is confirmed by endoscopic appearance and smooth passage of endoscope (8). With accumulation of experience and extension of indications, there are a few variations in technique across different centers in defining the GEJ and adequacy of myotomy, the optimal length, site of myotomy and whether the full thickness of the muscle wall should be cut.
Detection of GEJ & adequacy of myotomy
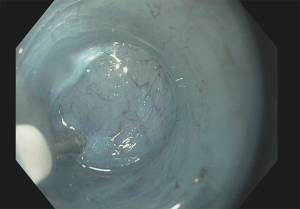
The gastric cardia is confirmed by (I) endoscopic measurements, (II) the opening up of submucosal space after passing the GEJ, (III) presence of palisading vessels (Figure 2), (IV) presence of larger calibre perforating vessels from the left gastric artery, (V) and the visualization of discolouration of submucosal tunnel from intraluminal view inside the stomach (14). Not all of these markers are accurate and clinically useful, especially in cases of sigmoidal esophagus where the length determined by endoscopy may be different from the actual distance due to the tortuosity of esophagus. Grimes et al. published a randomized controlled trial comparing the use of a second endoscope in detecting the transillumination from the end of the submucosal tunnel, viewing from a retroflex angle at the gastric cardia. The author concluded that using a second endoscope increased the procedure time by 17 min, but would lead to extension of the gastric myotomy length in 34% of patients (22). Minami et al. suggested injection of 0.5 mL of indocyanine green (ICG) into the lesser curvature of the gastric cardia prior to POEM as a tattoo to mark the end of the submucosal tunnel (19).
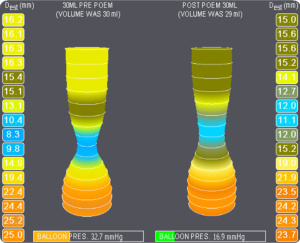
Another way to predict procedure endpoint in real-time intraoperatively is by the Endoluminal Functional Lumen Imaging Probe (EndoFLIP). EndoFLIP makes use of impedance planimetry to measure the diameter and cross-sectional area of EGJ. The intra-balloon pressure is also measured, and together, the distensibility of EGJ can be calculated. EGJ distensibility index (DI) was based on the narrowest cross-sectional area divided by the sum of intra-balloon pressure and intragastric pressure offset (23). Familiari et al. reported 23 patients using EndoFLIP for intraoperative evaluation of GEJ diameter during POEM. One patient was found to have suboptimal opening diameter of GEJ after initial completion of myotomy and therefore further myotomy was performed (24). Teitelbaum et al. demonstrated that submucosal tunnelling itself would increase the DI from 1.2 to 3.6 mm2/mmHg and 2 cm gastric myotomy would further increase the DI to 7.2 mm2/mmHg. EndoFLIP therefore provides an intraoperative tool in monitoring the completeness of myotomy and the effect of operation (25). Teitelbaum et al. suggested an ideal range of DI (4.5-8.5 mm2/mmHg) can achieve optimal symptoms control while minimizing complication of reflux (26) (Figure 3).
Length and site of myotomy
The conventional POEM myotomy length averages 8 to 10 cm. Its efficacy is reported in the literature. Depending on the indication, the proximal limit of the myotomy can be extended. In a systemic review and meta-analysis by Khan et al. on POEM for spastic esophageal disease, the mean length for submucosal tunnel was 17.2 cm and the length of myotomy was 13.5 cm (13). It is especially important as the pathophysiology of spastic esophageal disorder is caused by abnormal contractions in the esophageal body. The length of myotomy can be tailored according to preoperative investigation. Hoppo et al. have given examples of patients with previous myotomy or POEM where preoperative high resolution manometry or contrast study demonstrated the location of residual hypercontractility. The subsequent POEM can target at these lesions to eliminate persistent esophageal contractions. The group also attempted hybrid procedure with laparoscopic fundoplication with long POEM extending to proximal esophagus in selected cases (27).
Endoscopists also vary in preference on the location of myotomy. The original POEM utilized an anterior/2 o’clock/lesser curvature myotomy, mimicking the surgical procedure. It also avoids disrupting the angle of His and therefore theoretically minimizes the chance of postoperative reflux. Some operators prefer the posterior/7 o’clock/greater curvature myotomy. This path may have different flow-dynamics to reduce the amount of reflux during gastric contraction; the line of myotomy goes along the spine and provides a straighter submucosal tunnel in sigmoidal esophagus. In patients with previous anterior myotomy, it can provide a virgin plane (8,9,18,19). There is not enough evidence to recommend one over the other, currently it depends on endoscopists’ preference, except in re-do patients to avoid previous site of myotomy.
Full thickness vs. circular muscle myotomy
Inoue et al. advocated precise dissection of the circular muscle bundle with triangle-tip knife (8). Some other centers prefers full thickness myotomy because the plane between circular and longitudinal muscle is not always clear and is often obscured near the GEJ and beyond. Attempting to preserve the thin longitudinal muscle fibre may cause incomplete circular myotomy. The procedure is also considered to be simpler and faster (18). A retrospective study comparing the outcomes of full-thickness and circular muscle myotomy showed the mean operative time was significantly shorter in the full-thickness group and there was no increase in procedural related adverse event (28).
Efficacy & complication
Inoue et al. has published promising long-term results of the first 500 cases with success rate of 91% in 1–2 years and 88.5% in 3 years. Is this reproducible in other parts of the world? A meta-analysis involving 36 studies and 2373 patients was published recently. Asian countries have dominated the number of procedures by contributing around 63% of the patients. The clinical success rate was achieved in 98%, however the follow-up period was not specified. Excluding gas-related complications, the most common procedure-related adverse event was mucosal injury (4.8%).
The most concerned long-term complication of POEM is gastroesophageal reflux disease (GERD); unlike laparoscopic Heller myotomy, an anti-reflux procedure is not added. Depending on the parameters of GERD assessment, the incidence varies. In the meta-analysis, abnormal acid exposure in 24-hour pH monitoring is as high as 47%, while if only symptomatic GERD is considered, the incidence is 8.5%. Esophagitis occurs in 13% of patients when endoscopic examination is carried out (29). Familiari et al. reported that in 50.5% patients, abnormal acid exposure was found and clinically relevant GERD was evident in 29.1%. Esophagitis and symptoms resolved completely with proton pump inhibitor (30).
Despite the high success rate of POEM, evidence from head-to-head comparison to laparoscopic Heller myotomy, is lacking. The recruitment of in a randomized controlled trial comparing endoscopic versus laparoscopic myotomy for achalasia has been completed. It aimed to recruit 240 patients from Czech Republic, Germany, Italy, Netherlands and Sweden. The estimated study completion date would be in December 2019. Before that, there are several systematic reviews and meta-analyses based on retrospective data published in recent years. Talukdar et al. concluded that there were no differences between POEM and laparoscopic myotomy in reduction of Eckardt score, postoperative pain, length of hospital stay, adverse events and symptomatic GERD. Operative time was significantly lower for POEM (31). Marano et al. systematically reviewed data of 486 patients (196 in POEM group and 290 in laparoscopic myotomy group). The study showed that there were no differences in clinical response, operative time, postoperative pain and adverse event. The length of hospital stay was found to be shorter for POEM. However symptomatic gastroesophageal reflux rate was in favor of laparoscopic myotomy compared to POEM (32). It is obvious that with the current retrospective, non-randomized nature of the included studies, the evidence is conflicting and inconclusive. But the clinical advantage of POEM is obvious, and this advantage extends beyond the usual indications, patient group and patients with prior treatments.
Future & beyond
The popularity of POEM has led to development of more procedures possible with submucosal tunnelling. Peroral endoscopic tumour resection (POET) or submucosal tunnelling endoscopic resection (STER) is now adopted in many centers to resect submucosal tumour. For tumour arising from the muscularis propria, direct endoscopic resection or snaring would result in full thickness perforation. Tunnelling provides safety by offsetting the site of mucosal entry and site of tumor resection. Size of the tumour would potentially limit the removal of the mass using this technique, though in expert centers sizable tumor removal has been reported (10).
Another procedure inspired by POEM is antropyloromyotomy (G-POEM) in the treatment of gastroparesis. The pathophysiology of gastroparesis included alteration of gastric motility and increase in pyloric tone. The common causes included diabetes, post-surgical condition (such as after esophagectomy) and idiopathic. Gonzalez et al. reported a series of 12 patients with G-POEM and attained 100% technical success rate; 85% of patient achieved clinical improvement (33).
POEM has stimulated the field of submucosal tunnel endoscopy. Eleftheriadis et al. suggested some future perspectives in the indication of NOTES, such as endoscopic vagotomy, thoracoscopy, retroperitoneoscopy, peritoneoscopy and sympathectomy (10). The future is undeniably exciting.
Conclusions
Since its introduction in 2008, POEM has gained popularity in the treatment of achalasia and other esophageal motility disorders worldwide. It has provided a new option for a wide range of patients. Overwhelming literatures have demonstrated its efficacy and safety. Although comparative randomized control trials are still undergoing, it probably cannot stop the pendulum in shifting to this minimally invasive NOTES approach. GERD remains the weakest link as a complication of POEM, but after all, it is readily treatable by proton pump inhibitor or an additional fundoplication. To date, the technique is still restricted to limited expert centers, the generalizability and learning curve of the procedure is yet to be defined. The future application of submucosal tunnelling is thrilling.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare
References
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160-74. [Crossref] [PubMed]
- Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24 Suppl 1:57-65. [Crossref] [PubMed]
- Tack J, Zaninotto G. Therapeutic options in oesophageal dysphagia. Nat Rev Gastroenterol Hepatol 2015;12:332-41. [Crossref] [PubMed]
- Zerbib F, Roman S. Current Therapeutic Options for Esophageal Motor Disorders as Defined by the Chicago Classification. J Clin Gastroenterol 2015;49:451-60. [PubMed]
- Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA 2015;313:1841-52. [Crossref] [PubMed]
- Moonen A, Annese V, Belmans A, et al. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 2016;65:732-9. [Crossref] [PubMed]
- Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 2007;39:761-4. [Crossref] [PubMed]
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265-71. [Crossref] [PubMed]
- Inoue H, Sato H, Ikeda H, et al. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg 2015;221:256-64. [Crossref] [PubMed]
- Eleftheriadis N, Inoue H, Ikeda H, et al. Submucosal tunnel endoscopy: Peroral endoscopic myotomy and peroral endoscopic tumor resection. World J Gastrointest Endosc 2016;8:86-103. [Crossref] [PubMed]
- Youn YH, Minami H, Chiu PW, et al. Peroral Endoscopic Myotomy for Treating Achalasia and Esophageal Motility Disorders. J Neurogastroenterol Motil 2016;22:14-24. [Crossref] [PubMed]
- Khashab MA, Messallam AA, Onimaru M, et al. International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video). Gastrointest Endosc 2015;81:1170-7. [Crossref] [PubMed]
- Khan MA, Kumbhari V, Ngamruengphong S, et al. Is POEM the Answer for Management of Spastic Esophageal Disorders? A Systematic Review and Meta-Analysis. Dig Dis Sci 2017;62:35-44. [Crossref] [PubMed]
- Committee NPWP, Stavropoulos SN, Desilets DJ, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc 2014;80:1-15. [Crossref] [PubMed]
- Chen YI, Inoue H, Ujiki M, et al. An international multicenter study evaluating the clinical efficacy and safety of per-oral endoscopic myotomy in octogenarians. Gastrointest Endosc 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Chen WF, Li QL, Zhou PH, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: a prospective, single-center study. Gastrointest Endosc 2015;81:91-100. [Crossref] [PubMed]
- Nabi Z, Ramchandani M, Reddy DN, et al. Per Oral Endoscopic Myotomy in Children with Achalasia Cardia. J Neurogastroenterol Motil 2016;22:613-9. [Crossref] [PubMed]
- Hu JW, Li QL, Zhou PH, et al. Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: long-term outcomes from a prospective, single-center study. Surg Endosc 2015;29:2841-50. [Crossref] [PubMed]
- Minami H, Inoue H, Haji A, et al. Per-oral endoscopic myotomy: emerging indications and evolving techniques. Dig Endosc 2015;27:175-81. [Crossref] [PubMed]
- Stavropoulos SN, Modayil RJ, Friedel D, et al. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc 2013;27:3322-38. [Crossref] [PubMed]
- Ngamruengphong S, Inoue H, Ujiki MB, et al. Efficacy and Safety of Peroral Endoscopic Myotomy for Treatment of Achalasia after Failed Heller Myotomy. Clin Gastroenterol Hepatol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Grimes KL, Inoue H, Onimaru M, et al. Double-scope per oral endoscopic myotomy (POEM): a prospective randomized controlled trial. Surg Endosc 2016;30:1344-51. [Crossref] [PubMed]
- Kwiatek MA, Pandolfino JE, Hirano I, et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 2010;72:272-8. [Crossref] [PubMed]
- Familiari P, Gigante G, Marchese M, et al. EndoFLIP system for the intraoperative evaluation of peroral endoscopic myotomy. United European Gastroenterol J 2014;2:77-83. [Crossref] [PubMed]
- Teitelbaum EN, Sternbach JM, El Khoury R, et al. The effect of incremental distal gastric myotomy lengths on EGJ distensibility during POEM for achalasia. Surg Endosc 2016;30:745-50. [Crossref] [PubMed]
- Teitelbaum EN, Soper NJ, Pandolfino JE, et al. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 2015;29:522-8. [Crossref] [PubMed]
- Hoppo T, Thakkar SJ, Schumacher LY, et al. A utility of peroral endoscopic myotomy (POEM) across the spectrum of esophageal motility disorders. Surg Endosc 2016;30:233-44. [Crossref] [PubMed]
- Li QL, Chen WF, Zhou PH, et al. Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 2013;217:442-51. [Crossref] [PubMed]
- Akintoye E, Kumar N, Obaitan I, et al. Peroral endoscopic myotomy: a meta-analysis. Endoscopy 2016;48:1059-68. [Crossref] [PubMed]
- Familiari P, Greco S, Gigante G, et al. Gastroesophageal reflux disease after peroral endoscopic myotomy: Analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc 2016;28:33-41. [Crossref] [PubMed]
- Talukdar R, Inoue H, Nageshwar Reddy D. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: a systematic review and meta-analysis. Surg Endosc 2015;29:3030-46. [Crossref] [PubMed]
- Marano L, Pallabazzer G, Solito B, et al. Surgery or Peroral Esophageal Myotomy for Achalasia: A Systematic Review and Meta-Analysis. Medicine (Baltimore) 2016;95:e3001. [Crossref] [PubMed]
- Gonzalez JM, Lestelle V, Benezech A, et al. Gastric per-oral endoscopic myotomy with antropyloromyotomy in the treatment of refractory gastroparesis: clinical experience with follow-up and scintigraphic evaluation (with video). Gastrointest Endosc 2017;85:132-9. [Crossref] [PubMed]