Laparoscopic and endoscopic cooperative surgery for gastrointestinal tumor
Introduction
Since the development of laparoscopic surgery, local resection can be performed using a laparoscopic linear staplers through small wounds for trocar sites. In particular, for subepithelial tumors (SETs) of the stomach such as gastrointestinal stromal tumors (GISTs), local resection is accepted because GIST rarely metastasizes to lymph nodes (1). Consequently, prophylactic lymphadenectomy for GIST is not required. Laparoscopic wedge resection is a less invasive treatment for SETs of the stomach (2). A surgical approach from the peritoneal cavity is sometimes difficult for intraluminal or intramural growth type of gastric SET because the tumors can’t be identified from the peritoneal cavity, although extramural growth type of gastric SETs can be cured easily by laparoscopic wedge resection. Thus, an unintentional large resection may result in deformity and malfunction of the remaining stomach, which potentially causes prolonged gastric emptying. This surgery can lead to a result in a positive surgical margin, and it cause subsequently tumor recurrence (3-5). Furthermore, this is not applied to gastric SETs located at the esophagogastric junction (EGJ) and pylorus, because it is difficult to resect a lesion located at the EGJ or pylorus using a linear stapling device. Endoscopic submucosal dissection (ESD) is widely known as an effective treatment for superficial gastrointestinal neoplasms. ESD enables en bloc complete resection of tumors, regardless of their location and size (6-8). With technological progress of ESD, endoscopic full-thickness resection (EFTR) techniques have been developed for gastric SETs (9-16). These techniques are advantageous because a resection line can be determined more precisely using endoluminal endoscopy. Hence, it is possible to minimize the resection area as much as possible and subsequent deformity of the stomach, and better secure the surgical margins. In the current review, recent developments related to LECS procedures for gastrointestinal tumor are presented and discussed.
Endoscopic and laparoscopic approach
The cooperation of endoscopists and laparoscopists is essential for implementation of LECS procedures. The basic endoscopic and laparoscopic approach for lesion is as follows: the lesion is recognized directly under endoscopic visualization and fully resected as an en bloc full-thickness fashion endoscopically and/or laparoscopically. The defect of the stomach wall is sutured by laparoscopic linear staplers or laparoscopic hand-suturing techniques. A minimal blood vessel treatment is desirable, because excessive blood vessel treatment may result in postoperative immobility of the stomach. This endoscopic and laparoscopic approach makes it possible to resect a lesion as small as possible and to preserve anatomical function of the stomach.
GISTs are mesenchymal tumors in the gastrointestinal tract and considered potentially malignant tumors. Most GISTs are usually detected by endoscopy as a SET. The standard treatment for GIST is en bloc complete resection that avoids rupture and damage to the pseudo-capsule of the tumor (17,18). Moreover, SETs with ulceration have a potential risk of tumor cell seeding into the abdominal cavity by communicating between endoluminal and extraluminal spaces. Accordingly, we should pay great attention to avoid tumor dissemination by communication of the tumor surface into the peritoneal cavity.
Hiki et al. first reported laparoscopic and endoscopic cooperative surgery (LECS), it is named classical LECS at the present moment (9). LECS for gastrointestinal tumor is mainly sorted by two categories: exposure procedures and non-exposure procedures, which means to communicate between endoluminal and extraluminal spaces or not. A previous study reported that 1×104–9×106 colony-forming units (CFU)/mL of bacteria were detected when the stomach juice was cultured (19). On the other hand, it was reported that perforation during ESD for early gastric cancer was not to lead to peritoneal seeding, even with long-term observation (20). Presently, it remains controversial. The exposure procedures would have the potential risk of gastric contents or tumor cells spilling out over the abdominal cavity because the stomach wall has to be opened during the procedure. Thus, their application is limited to SETs without ulceration, which may not increase the risk of peritoneal dissemination. To avoid these potential risks, non-exposure procedures has been developed. In the next section, we explain precisely classical LECS and several LECS-related procedures and summarize each procedure in Table 1.
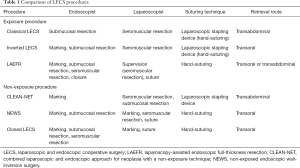
Full table
Classical LECS and LECS-related procedures
Exposure procedure
Classical LECS
Hiki et al. first reported this procedure (9). The specific procedure is described as follows. The tumor location from the serosal side is confirmed from the mucosal side by the tip of knife through the intraluminal endoscopy. After confirmation of the tumor location, muco-submucosal layers around the tumor are dissected circumferentially, performed by the ESD technique using intraluminal endoscopy. Subsequently, an artificial perforation of the seromuscular layer is made by the endoscopist using an ESD knife under instruction of the laparoscopist. The remaining seromuscular layer is dissected along the incision line made by the ESD technique both endoscopically and laparoscopically. After the tumor is resected completely, the gastric wall defect is sutured using a laparoscopic linear stapling device, and the tumor is removed transabdominally.
This procedure is simple and easy to introduce when endoscopists and laparoscopists have standard therapeutic skills. Classical LECS procedure can be surely and safely performed with reasonable operation time and adequate surgical margins. The advantages make it possible to resect a lesion as small as possible and less deformation of the stomach. However, this method contains intentional perforation of the stomach wall, which might cause bacterial contamination or tumor seeding into the abdominal cavity. Moreover, classical LECS for SETs located at the cardia requires a skillful technique to suture, because stenosis and leakage might be caused.
Inverted LECS
There are several drawbacks associated with classical LECS. Therefore, a LECS-related procedure, referred to as inverted LECS (10), was developed to prevent bacterial contamination or tumor dissemination. The procedure, from placing the markings to performing the artificial perforation, is almost the same as that of the classical LECS. To prevent the tumor contacting the visceral tissue and tumor cells spilling out over the peritoneal cavity, the stomach wall is pulled up circumferentially along the incision line as a crown using some stitches. Then, the seromuscular layer is circumferentially dissected using ESD knife or laparoscopic devices along the incision line of the submucosal layer. The tumor is resected completely and the specimen is retrieved perorally. Finally, the defect of gastric wall is sutured by laparoscopic linear staplers or laparoscopic hand-suturing technique.
The procedure was developed to prevent stomach contents from spilling out over the peritoneal cavity. The tumor is turned toward the intra-gastric cavity by two of the stitches, and the resection line is pulled up like a crown by several stitches. Accordingly, we can prevent stomach contents or tumor cells from spilling out over the peritoneal cavity and the tumor from contacting with visceral tissue. However, the procedure by traction on the stitches is to some extent complex, and there is still a risk of gastric content or tumor cells contamination since the gastric lumen is opened to the peritoneal cavity.
LAEFR
EFTR enables en bloc full-thickness resection of lesions with a minimum surgical margin. Pure EFTR, without laparoscopic procedures, has attracted attention as an extremely minimally invasive treatment. Abe et al. first reported full-thickness resection for gastric cancer under laparoscopic and endoscopic guidance, named as laparoscopy-assisted endoscopic full-thickness resection (LAEFR) (11,12). The specific procedure is described as follows. After a circumferential muco-submucosal layer around the lesion is incised, seromuscular layers are dissected not laparoscopically but endoscopically to the greatest possible extent under laparoscopic supervision. The gastric wall is stretched laparoscopically in order to make it easier for the endoscopist to perform seromuscular incision endoscopically. The specimen is retrieved perorally or transabdominally. Seromuscular incision and a suture for the stomach wall defect are performed endoscopically as much as possible instead of laparoscopic linear staplers.
LAEFR enables full-thickness resection of the lesions as small as possible only endoscopically under laparoscopic supervision. However, once perforation occurs, the endoscopic view is different from that of the usual ESD, and the appropriate dissection line becomes difficult to determine in the endoscopic seromuscular dissection. Therefore, LAEFR is a little complicated procedure and requires a skillful endoscopists’s technique. Furthermore, gastric wall is completely opened to the peritoneal cavity. Gastric contents flow and contaminate the peritoneal cavity to some degree. In addition, LAEFR can be applicable to a tumor located adjacent to the EGJ or the pyloric ring, which is technically difficult by laparoscopic wedge resection, although this procedure for a lesion located at the posterior wall of the EGJ would be extremely challenging. There are several problems which should be solved, such as the need for a full-thickness suturing device endoscopically and a counter traction device to create a good surgical field in the endoscopic seromuscular dissection.
Non-exposure procedure
Combined laparoscopic and endoscopic approach for neoplasia with a non-exposure technique (CLEAN-NET)
Inoue et al. invented and reported the CLEAN-NET for gastric neoplasms (13). CLEAN-NET enables full-thickness resection of the stomach without spilling a drop of gastric contents into the peritoneal cavity. Therefore, this procedure can be a less invasive surgery for gastric lesions without a risk of bacterial contamination or tumor seeding into the peritoneal cavity.
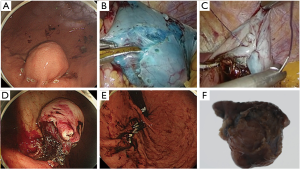
The specific procedure is described as follows. After marking around the lesion, the mucosal layer is fastened to the seromuscular layer with stitches using stay sutures, which is performed with laparoscopic guidance. By using a seromuscular incision, mucosa that surrounds the full-layer specimen can be stretched and maintain a sufficient margin around the tumor tissue. And then, by pulling stitches upward with laparoscopic forceps, selective seromuscular dissection outside the stitches is performed using a laparoscopic linear stapling device. The lesion is retrieved transabdominally (Figure 1).

The mucosal layer can be pulled up easily toward the abdominal cavity by seromuscular incision laparoscopically, and the stretched mucosa can be dissected with a minimal surgical margin. In the original article, a specimen and mucosa surrounding the lesion are lifted by four stay sutures. If the mucosal tissue could be pulled up enough toward the outside of the stomach, lift by four stay sutures might be unnecessary. Although this technique is attractive in terms of technical accessibility, full-layer resection using a mechanical stapler is blindly performed without exposing the mucosal surface to the peritoneal cavity. Therefore, CLEAN-NET has potential risk of margin positive or larger resection size than expected.
NEWS
Goto et al. invented and reported the non-exposed endoscopic wall-inversion surgery (NEWS) (14,15). NEWS is an effective full-thickness resection with a minimum possible margin without bacterial contamination and tumor seeding into the abdominal cavity. The specific procedure is described as follows. After markings of mucosal and serosal side, circumferential seromuscular layers incision are made laparoscopically. The seromuscular layers are linearly sutured, with the lesion and the spacer inverted inward the stomach. The spacer extends the space between the sutured seromuscular plane and the serosal surface of the inverted lesion, and facilitates the seromuscular dissection. Then, a circumferential muco-submucosal incision is made. Finally, the specimen is retrieved perorally (Figure 2).
This technique is considered as a minimally invasive and reliable full-thickness resection without risks of bacterial contamination or tumor seeding into the peritoneal cavity in patients with gastric tumors irrespective of ulceration, retrieved perorally. It would be optimal compared with ESD in terms of safety and certainty. However, this technique may be technically difficult to perform because it includes unique process both endoscopically and laparoscopically, such as serosal marking matched to the mucosal markings, seromuscular incision and suturing, and mucosal incision around the inverted lesion. Thus, NEWS might be a little complicated and time-consuming procedure. However, the recent report clarified that NEWS was successfully performed within an acceptable operation time without severe adverse events (15). It proves that NEWS would be technically acceptable.
Closed LECS
The concept of closed LECS is similar to that of NEWS (16); closed LECS is like NEWS without laparoscopic seromuscular incision. The specific procedure is described as follows. After mucosal markings, circumferential muco-submucosal incision around the tumor is made endoscopically using the ESD technique. And then, laparoscopic serosal markings are made matched to the muco-submucosal incision line under endoscopic guidance. Subsequently, a spongy spacer is put on the serosal surface and fixed at the center of the suture line by the suturing of both sides of the serosa, and continuous seromuscular suturing is performed in a way to bury the spacer. Finally, circumferential seromuscular dissection is performed with an ESD knife along the muco-submucosal incision line. The lesion is resected endoscopically, and the resected lesion is retrieved perorally.
The difference between closed LECS and NEWS is whether or not to perform laparoscopic circumferential seromuscular incision. In closed LECS, the seromuscular layers are resected blindly without checking the serosal side. Hence, it might be difficult to perform full-thickness resection securely.
Outcomes of classical LECS and LECS-related procedures
Published data are shown in Table 2 (9-16,21-24). The tumor size was 7–60 mm, and the resected specimen size was 22.7–80 mm. The operation time was 152–389 min, the blood loss was 0–177 mL, and the postoperative stay was 7–11.6 days. Most of the lesions were completely resected as en bloc fashion. There were no fatal complications. With this data considered, procedure time is acceptable, and blood loss is little. The lesions are resected completely in almost all cases. Furthermore, a precise diagnosis is made in all the specimens. The most significant advantage of LECS procedure is safer and securer than that of previous procedures. However, there seems to be technically difficulties to some extent in each procedure at the time of introduction.

Full table
Indication for LECS procedures
There are slight differences in indication for LECS procedures between SETs and gastrointestinal cancers (Table 3).

Full table
SETs
The indication criteria for LECS is SETs, regardless of the location, with a maximum diameter of 50 mm, according to the indications for laparoscopic resection of GISTs suggested by the National comprehensive Cancer Network (25) and Japanese guideline of GIST (26). In general, laparoscopic wedge resection for especially the extraluminal growth type gastric SETs can be performed easily, LECS is mainly performed for the intraluminal or intramural growth type SETs of the stomach.
SETs with ulceration have a potential risk of tumor seeding into the abdominal cavity by communicating between endoluminal and extraluminal spaces. The exposure procedure should be used for gastric SETs without ulceration, although the non-exposure procedure can be used for gastric SETs regardless of ulceration.
When the lesion is retrieved perorally, a maximum diameter of the lesion is limited within 30 mm. Moreover, when the lesion is resected with laparoscopic linear stapling device, the certain locations of the stomach (e.g., EGJ, pylorus, and lesser curvature) might be limited, because it is difficult for those locations to apply by a laparoscopic stapling device. In terms of tumor location, laparoscopic hand-suturing of the gastric wall defect is more desirable than that of laparoscopic linear staplers, although it is time-consuming procedure.
Gastrointestinal cancers
ESD is universally accepted as a less invasive curative treatment for early gastrointestinal cancer that enables the preservation of function and maintains the patients’ quality of life. However, ESD still requires a skilled operator especially for lesions located at the greater curvature of fornix and the upper body of the stomach, and for lesions with severe ulceration. ESD for these lesions has a higher probability of complications such as perforation and bleeding. Furthermore, it takes longer operation times to perform ESD. Therefore, LECS may be an alternative treatment option especially for lesions difficult to resect by ESD.
The most important point when treating gastrointestinal cancer is to prevent tumor cells seeding into the abdominal cavity. We should pay careful attention to avoid scattering of gastric contents or contacts between the tumor and the surrounding visceral tissue during the procedure. Therefore, it is desirable to use a non-exposure procedure to prevent bacterial contamination and peritoneal dissemination of tumor cells.
Recently, LECS has been performed not only for early gastric cancer but also for duodenal lesion. Although ESD has been presently performed for superficial nonampullary tumors in the duodenum (27), it is well noted that delayed perforation and bleeding occurs frequently after duodenal ESD (28,29). Moreover, this procedure cannot apply to periampullary tumors, because suturing of seromuscular layer cannot be performed near the pancreas. LECS has been reported for duodenal lesions, including early duodenal cancers or duodenal SETs, and the reports suggest that it is beneficial because of its minimal invasiveness and histological accuracy (30,31). However, the most appropriate treatment for duodenal lesions has not been fully established.
Future outlook of LECS
Sentinel node navigation surgery (SNNS) is expected technique that is able to diagnose lymph node metastasis intraoperatively. This concept enables us to minimize the resection area of lymphadenectomy and gastrectomy by detecting lymphatic flows (32,33). Presently, it remains controversial whether SNNS is feasible in EGC, although the feasibility of SNNS has been reported from several limited institutions (33). If SNNS is established, the indication for LECS of EGC could be expanded, and LECS with SNNS would provide a minimally invasive surgery for EGC in the future.
Conclusions
LECS is a minimally invasive and safe procedure, and would maintain subsequent patient’s quality of life by resecting a lesion with minimal margins and preserving anatomical function of the stomach. Especially, non-exposure LECS procedures are technically demanding, time-consuming, and even cost-ineffective so far, which would be overcame by the suitable devices in the future, these procedures are promising and patient-oriented in terms of minimally invasiveness, certainty and safety. At present, these reports are limited to case reports. Further studies such as a large number of prospective clinical studies are required to show the feasibility of these treatment procedures.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest(201hao to declare.
References
- Ma GL, Murphy JD, Martinez ME, et al. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiol Biomarkers Prev 2015;24:298-302. [Crossref] [PubMed]
- Otani Y, Ohgami M, Igarashi N, et al. Laparoscopic wedge resection of gastric submucosal tumors. Surg Laparosc Endosc Percutan Tech 2000;10:19-23. [Crossref] [PubMed]
- Ishikawa K, Inomata M, Etoh T, et al. Long-term outcome of laparoscopic wedge resection for gastric submucosal tumor compared with open wedge resection. Surg Laparosc Endosc Percutan Tech 2006;16:82-5. [Crossref] [PubMed]
- Kitano S, Shiraishi N. Minimally invasive surgery for gastric tumors. Surg Clin North Am 2005;85:151-64. xi. [Crossref] [PubMed]
- Lee JH, Han HS, Kim YW, et al. Laparoscopic wedge resection with handsewn closure for gastroduodenal tumors. J Laparoendosc Adv Surg Tech A 2003;13:349-53. [Crossref] [PubMed]
- Goto O, Fujishiro M, Kodashima S, et al. Outcomes of endoscopic submucosal dissection for early gastric cancer with special reference to validation for curability criteria. Endoscopy 2009;41:118-22. [Crossref] [PubMed]
- Ono S, Fujishiro M, Niimi K, et al. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc 2009;70:860-6. [Crossref] [PubMed]
- Niimi K, Fujishiro M, Kodashima S, et al. Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 2010;42:723-9. [Crossref] [PubMed]
- Hiki N, Yamamoto Y, Fukunaga T, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc 2008;22:1729-35. [Crossref] [PubMed]
- Nunobe S, Hiki N, Gotoda T, et al. Successful application of laparoscopic and endoscopic cooperative surgery (LECS) for a lateral-spreading mucosal gastric cancer. Gastric Cancer 2012;15:338-42. [Crossref] [PubMed]
- Abe N, Mori T, Takeuchi H, et al. Successful treatment of early stage gastric cancer by laparoscopy-assisted endoscopic full-thickness resection with lymphadenectomy. Gastrointest Endosc 2008;68:1220-4. [Crossref] [PubMed]
- Abe N, Takeuchi H, Yanagida O, et al. Endoscopic full-thickness resection with laparoscopic assistance as hybrid NOTES for gastric submucosal tumor. Surg Endosc 2009;23:1908-13. [Crossref] [PubMed]
- Inoue H, Ikeda H, Hosoya T, et al. Endoscopic mucosal resection, endoscopic submucosal dissection, and beyond: full-layer resection for gastric cancer with nonexposure technique (CLEAN-NET). Surg Oncol Clin N Am 2012;21:129-40. [Crossref] [PubMed]
- Mitsui T, Niimi K, Yamashita H, et al. Non-exposed endoscopic wall-inversion surgery as a novel partial gastrectomy technique. Gastric Cancer 2014;17:594-9. [Crossref] [PubMed]
- Goto O, Takeuchi H, Sasaki M, et al. Laparoscopy-assisted endoscopic full-thickness resection of gastric subepithelial tumors using a nonexposure technique. Endoscopy 2016;48:1010-5. [Crossref] [PubMed]
- Kikuchi S, Nishizaki M, Kuroda S, et al. Nonexposure laparoscopic and endoscopic cooperative surgery (closed laparoscopic and endoscopic cooperative surgery) for gastric submucosal tumor. Gastric Cancer 2017;20:553-7. [PubMed]
- Nishida T, Blay JY, Hirota S, et al. The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer 2016;19:3-14. [Crossref] [PubMed]
- ESMO/European Sarcoma Network Working Group. Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2014;25 Suppl 3:iii21-6. [Crossref] [PubMed]
- Mori H, Kobara H, Tsushimi T, et al. Reduction effect of bacterial counts by preoperative saline lavage of the stomach in performing laparoscopic and endoscopic cooperative surgery. World J Gastroenterol 2014;20:15763-70. [Crossref] [PubMed]
- Ikehara H, Gotoda T, Ono H, et al. Gastric perforation during endoscopic resection for gastric carcinoma and the risk of peritoneal dissemination. Br J Surg 2007;94:992-5. [Crossref] [PubMed]
- Tsujimoto H, Yaguchi Y, Kumano I, et al. Successful gastric submucosal tumor resection using laparoscopic and endoscopic cooperative surgery. World J Surg 2012;36:327-30. [Crossref] [PubMed]
- Hoteya S, Haruta S, Shinohara H, et al. Feasibility and safety of laparoscopic and endoscopic cooperative surgery for gastric submucosal tumors, including esophagogastric junction tumors. Dig Endosc 2014;26:538-44. [Crossref] [PubMed]
- Matsuda T, Hiki N, Nunobe S, et al. Feasibility of laparoscopic and endoscopic cooperative surgery for gastric submucosal tumors (with video). Gastrointest Endosc 2016;84:47-52. [Crossref] [PubMed]
- Niimi K, Aikou S, Kodashima S, et al. Video of the Month: A Novel Endoscopic Full-Thickness Resection for Early Gastric Cancer. Am J Gastroenterol 2015;110:1535. [Crossref] [PubMed]
- Demetri GD, von Mehren M, Antonescu CR, et al. NCCN Task Force report: update on the management of patients with gastrointestinal stromal tumors. J Natl Compr Canc Netw 2010;8 Suppl 2:S1-41; quiz S42-4.
- Nishida T, Hirota S, Yanagisawa A, et al. Clinical practice guidelines for gastrointestinal stromal tumor (GIST) in Japan: English version. Int J Clin Oncol 2008;13:416-30. [Crossref] [PubMed]
- Honda T, Yamamoto H, Osawa H, et al. Endoscopic submucosal dissection for superficial duodenal neoplasms. Dig Endosc 2009;21:270-4. [Crossref] [PubMed]
- Inoue T, Uedo N, Yamashina T, et al. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc 2014;26:220-7. [Crossref] [PubMed]
- Hoteya S, Kaise M, Iizuka T, et al. Delayed bleeding after endoscopic submucosal dissection for non-ampullary superficial duodenal neoplasias might be prevented by prophylactic endoscopic closure: analysis of risk factors. Dig Endosc 2015;27:323-30. [Crossref] [PubMed]
- Abe N, Takeuchi H, Hashimoto Y, et al. Laparoscopy-assisted transduodenal excision of superficial non-ampullary duodenal epithelial tumors. Asian J Endosc Surg 2015;8:310-5. [Crossref] [PubMed]
- Hirokawa F, Hayashi M, Miyamoto Y, et al. Laparoscopic and endoscopic cooperative surgery for duodenal tumor resection. Endoscopy 2014;46 Suppl 1 UCTN:E26-7.
- Takeuchi H, Kitagawa Y. New sentinel node mapping technologies for early gastric cancer. Ann Surg Oncol 2013;20:522-32. [Crossref] [PubMed]
- Kitagawa Y, Takeuchi H, Takagi Y, et al. Sentinel node mapping for gastric cancer: a prospective multicenter trial in Japan. J Clin Oncol 2013;31:3704-10. [Crossref] [PubMed]


