How to establish a successful ex vivo lung perfusion program
Introduction
Lung transplant is the ultimate solution for patients with end stage respiratory failure. The number of patients awaiting transplant continues to rise, and waitlist mortality is a growing concern due to the donor lung shortage (1-3). Donor lungs are subjected to several injurious mechanisms during the brain death/organ donation process (such as ventilator-acquired pneumonia, neurogenic and hydrostatic pulmonary edema, barotrauma, etc.) (2). Because of this, the majority of offered lungs are not used; only 15–20% of offered lungs are currently utilized (4-6). Expansion of the donor pool has been accomplished utilizing extended criteria donors, donation after cardiac death (DCD), and aggressive use of ECMO post-transplantation for marginal lungs (6-9). With the use of ex vivo lung perfusion (EVLP), even “more marginal” lungs can be assessed in an ex vivo setting prior to transplantation. By doing so, lungs that are deemed acceptable for implantation will expand the donor pool while those lungs that are deemed unacceptable and discarded and will help preserve or potentially improve outcomes. The EVLP is used in high-risk donor lungs which are defined as those meeting any one of the following criteria: (I) best ratio of the partial pressure of arterial oxygen (PaO2) to fraction of inspired oxygen (FIO2) of less than 300 mmHg; (II) pulmonary edema, defined as bilateral interstitial infiltrates without evidence of infection, detected on the last chest radiograph by the lung-transplantation physician assessing the donor; (III) poor lung deflation or inflation during direct intraoperative visual examination at the donor site; (IV) blood transfusions exceeding 10 units; (V) DCD (2,10).
Donor lungs with established pneumonia, severe mechanical lung injury (i.e., contusions in more than one lobe), or gross gastric aspiration were excluded (10).
EVLP has emerged as a valuable potential alternative to address this issue by utilizing a preservation technique that allows for more accurate lung assessment and possible improvement of lung function (2). The concept of EVLP is not only to evaluate lungs before transplantation, but also to recondition lungs of inferior quality outside the cadaver and to extend the total cold ischemic time by intermittent warm reperfusion (11). Early outcomes have been reported in recipients who underwent transplantation after EVLP to those with conventionally selected and transplanted lungs (11-14).
Discussion
Here we discuss how to establish a successful EVLP program by in seven steps (15), we carefully considered various factors which are important in implantation this technology step by step focusing on liaison, logistics, and organization, a number of recommendations have particular relevance to the American situation, but it could be used as a road map or a guidance for different national health care systems too.
Step 1: identify the need for an EVLP program
Being realistic is a key to success. Hospital administration should ensure that they have the resources, but you need to be sure that the program will succeed. You need to evaluate the potential number of EVLP cases you might be able to perform, as an EVLP program might not be a cost effective. You should also be willing to accept marginal lungs and be comfortable with the possibility that the lungs might not be suitable for transplant after mobilizing resources and time spent by your team. The preferable scenario is one in which a program has sufficient volume, and a robust waiting list.
Step 2: identify the physician leadership team
This includes Physician champions in the form of a qualified lung transplant surgeon and lung transplant pulmonologist; both will need to be willing to sacrifice sufficient time and efforts to proceed with this labor-intensive endeavor. Both need to have enough knowledge and master their subject as they will be the reference for all team members and the primary decision makers. Theses project champions will continuously oversee the program, periodically reassess and manage patient selections, and ensure high quality outcomes. They also need to critically analyze policies, training, annual competencies and recommend restructuring when indicated.
Step 3: receive support from the hospital leadership
In order to start an EVLP program, it is essential to have full administration support in order to secure start-up capital investment. The administration should understand the purpose of the program and be willing to invest continuing support to the project as the return on investment may not occur immediately. You will need to perform a cost analysis and the impact that EVLP would have on transplant program. The analysis should include the cost of purchasing disposable EVLP materials, staff salary, estimated call cost, and continuous training and education as well as scheduled maintenance. Key points in persuading your administration to commit the start-up capital would include the potential for more transplants and associated down-stream revenue, marketability, and increased visibility of the program to patients and referring physicians. These are some tips for engaging leaders in your project (16,17).
- Understand your leader’s style: know the personality of the person to whom you are trying to “sell” the idea or program to is critical to success. You need to find out what convinces the leader; numbers or stories;
- Find the best pathway to the administration: try to build a cross-disciplinary team (guiding coalition) of other department leaders, hospital frontline staff, patients and families who support the work. Within the group some people who have credibility with others, these people are volunteer to help (17). Having these diverse voices of support will build leverage for getting leadership buy-in;
- Be sure to establish a clear, ambitious vision that can inspire: talk about both the short-term and long-term implications of the initiative. Use evidence and experts to make your case, providing excellence can only be done by using evidence-based practices. Leaders want to know you have done your homework before committing resources to a new project, in general initial impressions are very strong and they can be hard to counteract;
- Align with external priorities: leadership is more likely to support a project that aligns with the future of their field. Appeal to your leaders by aligning your initiative with national priorities, especially those that are cutting edge;
- Communicate: by using all channels as (meeting, emails, one on one conversations). Getting administration buy-in is only half the battle. They still needed the go-ahead from leadership to fund the project once leaders are onboard with a project, it’s important to frequently share information to help transition them from supportive to engaged (18).
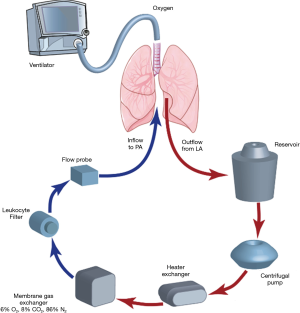
Step 4: build your own circuit to establish proficiency
An EVLP circuit can be built utilizing components available from the perfusion and respiratory departments of your institution. The basic components of an EVLP circuit include a ventilator, endotracheal tube, perfusion solution, tubing pack, reservoir, oxygenator, air filter, and pump. An O2 sensor is helpful but not mandatory. In addition, a tank of “de-oxygenating gas” is necessary to simulate O2 consumption by the circuit. Cannulas for the pulmonary artery and left atrial cuff are commercially available as are many of the above-mentioned components (Figure 1).
Step 5: identify your clinical team
Staffing of the circuit can take many forms. These employees will become staff level champions. These should include individuals with knowledge of perfusion, ventilator management, and arterial blood gas (ABG) interpretation. In addition to a physician, this can include perfusionists, respiratory therapists, extracorporeal membrane oxygenation (ECMO) clinicians, transplant OR staff, and research coordinator. Engaging diverse staff throughout the planning, design, and implementation of program improvement strategies is critical to facilitating successful and lasting change.
At our institution, an extracorporeal membrane oxygenation respiratory therapist (clinician) (RT-ECMO) is the sole staffing individual for an EVLP. This model was chosen because these individuals have an understanding of perfusion, ventilator management, and ABG interpretation. We have identified two people from day shift and two people from night shift for this position as one of them are in-house greater than 90% of the year. They are listed on our transplant call schedule and readily available on short notice for any clinical perfusion. They are supervised during an EVLP by a lung transplant physician.
Step 6: establish your staffing and training model
At present, EVLP is an infrequent event when compared to lung transplant. Once these components and individuals are in place, it is helpful to utilize a structured competency model of mock loops and non-human lungs to become familiar with the technique of EVLP. If non-human lungs are used, it is imperative to receive institutional review board (IRB) and Institutional Animal Care and Use Committee (IACUC) approval from your institution. Again, this will require institutional support in the form of compensation for educational time of your staff. You should also anticipate and address the staff resistance and culture change, continuous education is a key point for success. Off note whenever you start a new process, you always find that the time you’ve allocated for education is not enough.
Step 7: purchase your machine
Select the more convenient type of EVLP to your institution considering the above will be helpful in achieving a smooth transition to clinical application in a lung transplant program.
Summary
EVLP is becoming more prevalent and accepted technology in the armamentarium of lung transplantation. The key to any successful EVLP program is having a coordinated team of professionals who dedicate a significant portion of their time to the program. In order to start an EVLP program, it is essential that sufficient institutional support and staffing be available. Once established, it is imperative that ongoing training and proficiency methods are in place in order to assure optimal results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Popov AF, Sabashnikov A, Patil NP, et al. Ex vivo lung perfusion - state of the art in lung donor pool expansion. Med Sci Monit Basic Res 2015;21:9-14. [Crossref] [PubMed]
- Machuca TN, Cypel M. Ex vivo lung perfusion. J Thorac Dis 2014;6:1054-62. [PubMed]
- Valapour M, Paulson K, Smith JM, et al. OPTN/SRTR 2011 Annual Data Report: lung. Am J Transplant 2013;13 Suppl 1:149-77. [Crossref] [PubMed]
- Punch JD, Hayes DH, LaPorte FB, et al. Organ donation and utilization in the United States, 1996-2005. Am J Transplant 2007;7:1327-38. [Crossref] [PubMed]
- Van Raemdonck D, Neyrinck A, Verleden GM, et al. Lung donor selection and management. Proc Am Thorac Soc 2009;6:28-38. [Crossref] [PubMed]
- Yeung JC, Cypel M, Waddell TK, et al. Update on donor assessment, resuscitation, and acceptance criteria, including novel techniques--non-heart-beating donor lung retrieval and ex vivo donor lung perfusion. Thorac Surg Clin 2009;19:261-74. [Crossref] [PubMed]
- Cypel M, Keshavjee S. Strategies for safe donor expansion: donor management, donations after cardiac death, ex-vivo lung perfusion. Curr Opin Organ Transplant 2013;18:513-7. [Crossref] [PubMed]
- Van Raemdonck DE, Rega FR, Neyrinck AP, et al. Non-heart-beating donors. Semin Thorac Cardiovasc Surg 2004;16:309-21. [Crossref] [PubMed]
- Pierre AF, Sekine Y, Hutcheon MA, et al. Marginal donor lungs: a reassessment. J Thorac Cardiovasc Surg 2002;123:421-7;discussion, 427-8. [Crossref] [PubMed]
- Cypel M, Yeung JC, Liu M, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med 2011;364:1431-40. [Crossref] [PubMed]
- Wierup P, Haraldsson A, Nilsson F, et al. Ex vivo evaluation of nonacceptable donor lungs. Ann Thorac Surg 2006;81:460-6. [Crossref] [PubMed]
- Cypel M, Yeung JC, Machuca T, et al. Experience with the first 50 ex vivo lung perfusions in clinical transplantation. J Thorac Cardiovasc Surg 2012;144:1200-6. [Crossref] [PubMed]
- Aigner C, Slama A, Hötzenecker K, et al. Clinical ex vivo lung perfusion--pushing the limits. Am J Transplant 2012;12:1839-47. [Crossref] [PubMed]
- Inci I, Schuurmans MM, Boehler A, et al. Zurich University Hospital lung transplantation programme: update 2012. Swiss Med Wkly 2013;143:w13836. [PubMed]
- Wozniak TC. How Do You Start an EVLP Program? Available online: http://webcast.aats.org/2015/Presentations_2/608/04252015/1000-Optimal%20Therapi1/1130_Wozniak_T/How%20do%20you%20start%20an%20EVLP%20program_424.pdf
- Gallo A. How to Get Your Idea Approved. Available online: https://hbr.org/2010/11/how-to-get-their-approval.html
- Hutter C. 8 Tips for Engaging Leaders in Your Project. Available online: http://nichq.org/blog/2015/march/qitips_leadershipengagement
- Kotter JP, Whitehead LA. Buy-In: Saving Your Good Idea from Getting Shot Down. Boston: Harvard Business Review Press, 2010.