Meta-analysis on extracorporeal life support during cardiac arrest: do not compare apples and oranges
In a recent issue of Intensive Care Medicine, Ouweneel et al. provided a meta-analysis on extracorporeal life support (ECLS) during cardiac arrest (CA) and cardiogenic shock (1). Cardiogenic shock analysis compared ECLS vs. Impella, TandemHeart, or intra-aortic balloon pump (IABP). As these devices have various support levels, different specifications, and therefore different clinical indications, results issued from this analysis are clinically questionable. In addition, based on the recent IABP Shock II trial (2), current European guidelines on cardiogenic shock no longer support routine IABP therapy use, except for mechanical complications (class IIaC). As reported by the authors, caution is required in interpreting this part of the meta-analysis and our interest was therefore focused on the evaluation of ECLS during CA.
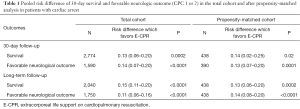
ECLS on cardiopulmonary resuscitation (E-CPR) is the ultimate rescue therapy, which might be offered only when conventional resuscitation measures have failed. Latest guidelines from the American Heart Association (AHA) (3) recommend that E-CPR should be considered “when ECPR is readily available, (…) the time without blood flow is short and the condition leading to CA is deemed reversible or amenable to heart transplantation or revascularization” (class IIb). As stated in this recommendation by a level of evidence at C, studies supporting these guidelines are actually limited (4-6). Most of them had small numbers of patients, and unbalanced comparison groups with respect to age, witness status, bystander CPR, and the quality of conventional CPR. In this setting, Ouweneel et al. gathered these heterogeneous studies and their meta-analysis brings new insights although no prospective randomized controlled trials exist yet. They selected nine retrospective studies (4,7-14), comparing E-CPR vs. conventional CPR (C-CPR), resulting in a total of 3.098 patients (708 ECLS vs. 2.390 control). Outcomes were 30-day survival rate and favorable neurological outcomes [Glasgow-Pittsburgh cerebral-performance categories (CPC) score of 1 or 2] at 30 days evaluated by total cohort and propensity-matched cohort analysis (when available). The usage of ECLS in this setting was associated with increased survival at 30 days (absolute risk difference 13%; 95% CI 6–20%; P>0.001) and higher rate of favorable neurological outcome at both 30 days (risk difference 14%; 95% CI 7–20%; P>0.001) and during long-term follow-up. Same tendencies were observed with propensity score matching (Table 1).
Full table
As mentioned by the authors, total-cohort analysis results should be taken with precaution and warrant discussion. First, all studies included CA patients with different inclusion criteria such as in-hospital cardiac arrest (IHCA), out-of-hospital cardiac arrest (OHCA), witnessed or non-witnessed CA and differing duration of CPR. Overall, ECLS patients were more likely to be younger, male, suffer from myocardial infarction and to undergo primary percutaneous coronary intervention (PCI). Second, the total-cohort analysis of survival rate is driven by Lee et al.’s cohort (10) (34% of total patients population included) whose E-CPR and C-CPR patients’ characteristics were significantly different in term of age, co-morbidities, CA’s location and cause and initial shockable rhythm (P<0.0001). These relevant factors were consistently reported as risk factors in studies on C-CPR (15,16). Third, revascularization procedures were more frequent in the E-CPR groups in several studies (4,11), which is an important bias to consider. Indeed, it is worth remembering that PCI is associated with better survival, which is made possible by ECLS for the most severe patients. Lastly, this meta-analysis constantly mixes studies focused on IHCA (4,7,8,10) and OHCA (9-12) with obviously very different survival rates (17). In our opinion, IHCA and OHCA have such distinct presentation, management delays, and outcome that mixing these two populations preclude raising any solid clinical message on E-CPR use. For the same reasons, neurological outcome in the total-cohort analysis is biased. Although it’s impact on neurological outcome remains uncertain (especially in the absence of an initial shockable rhythm) (18), hypothermia also differed between studies, introducing another potential confounding bias.
In absence of randomized controlled trial on this topic, propensity-matched support analysis where the propensity score reflects the probability of receiving ECLS therapy, could minimize these biases. Herein, 438 and 195 patients were matched for 30-day survival and neurological outcome evaluation, respectively (4,7,9,11,14). Despite a major reduction in the number of included patients, results remain in favor of E-CPR group for both 30-day survival rates (risk difference 14%; 95% CI 2–25%; P=0.02; number needed to treat 7.1) and favorable neurological outcome (risk difference 13%; 95% CI 7–20%; P=0.0001; NNT 7.7) (Table 1). These results were consistent with long-term outcomes. However, substantial heterogeneity (I2 =54%) was reported in this analysis. That was mainly explained by the study of Shin et al. (14) where PCI and return of spontaneous circulation (ROSC) were significantly more frequent in the E-CPR group (P<0.001 and P=0.004, respectively) and consequently weighted in the analysis with a higher risk difference (0.25; 95% IC 0.10–0.43). Lastly, although the number of patients included in the propensity-matched support analysis was limited, the most interesting result were obtained for 30-day and long-term neurological outcome evaluation, which remain in favor of the E-CPR group. However, it is worth pointing out that favorable neurological was observed only in 23% and 14% patients at 30 days and after long-term follow-up, respectively. In regard of this outcome, performing a secondary analysis aimed at differentiating between IHCA and OHCA would have been of interest to enable a more thorough interpretation of results. However, the small number of patients in each group would have unfortunately, limited this analysis.
In the context of E-CPR, the Pygmalion effect (or Rosenthal effect or self-fulfilling prophecy), phenomena whereby higher expectations lead to an increase in performance (19), has had a particular impact. Patients receiving E-CLS for CA are systematically younger with less co-morbidity. In this context, a full-code therapy which involves all stakeholders (pre-hospital team, mobile ECMO team, intensivists, nurses…) is more likely to be done. Indeed, patients who received E-CPR underwent more frequently PCI and hypothermia, which both may have an impact on the outcome. In the absence of randomized controlled trial, such propensity-matched analysis is still insufficient to evaluate the benefit of E-CPR vs. C-CPR. In the interim, E-CPR should be limited to refractory CA in young adults without comorbidities who received CPR from a bystander with a shockable rhythm. Ouweneel et al.’s meta-analysis pointed out the urgent need for a randomized controlled trial on this topic to determine which patients are likely to be the best candidates and how this costly rescue therapy should be performed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ouweneel DM, Schotborgh JV, Limpens J, et al. Extracorporeal life support during cardiac arrest and cardiogenic shock: a systematic review and meta-analysis. Intensive Care Med 2016;42:1922-34. [Crossref] [PubMed]
- Thiele H, Zeymer U, Neumann FJ, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med 2012;367:1287-96. [Crossref] [PubMed]
- Cave DM, Gazmuri RJ, Otto CW, et al. Part 7: CPR techniques and devices: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S720-8. [Crossref] [PubMed]
- Chen YS, Lin JW, Yu HY, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet 2008;372:554-61. [Crossref] [PubMed]
- Chen YS, Yu HY, Huang SC, et al. Extracorporeal membrane oxygenation support can extend the duration of cardiopulmonary resuscitation. Crit Care Med 2008;36:2529-35. [Crossref] [PubMed]
- Nagao K, Kikushima K, Watanabe K, et al. Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of-hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention. Circ J 2010;74:77-85. [Crossref] [PubMed]
- Blumenstein J, Leick J, Liebetrau C, et al. Extracorporeal life support in cardiovascular patients with observed refractory in-hospital cardiac arrest is associated with favourable short and long-term outcomes: A propensity-matched analysis. Eur Heart J Acute Cardiovasc Care 2016;5:13-22. [Crossref] [PubMed]
- Chou TH, Fang CC, Yen ZS, et al. An observational study of extracorporeal CPR for in-hospital cardiac arrest secondary to myocardial infarction. Emerg Med J 2014;31:441-7. [Crossref] [PubMed]
- Kim SJ, Jung JS, Park JH, et al. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care 2014;18:535. [Crossref] [PubMed]
- Lee SH, Jung JS, Lee KH, et al. Comparison of Extracorporeal Cardiopulmonary Resuscitation with Conventional Cardiopulmonary Resuscitation: Is Extracorporeal Cardiopulmonary Resuscitation Beneficial? Korean J Thorac Cardiovasc Surg 2015;48:318-27. [Crossref] [PubMed]
- Maekawa K, Tanno K, Hase M, et al. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med 2013;41:1186-96. [Crossref] [PubMed]
- Sakamoto T, Morimura N, Nagao K, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation 2014;85:762-8. [Crossref] [PubMed]
- Siao FY, Chiu CC, Chiu CW, et al. Managing cardiac arrest with refractory ventricular fibrillation in the emergency department: Conventional cardiopulmonary resuscitation versus extracorporeal cardiopulmonary resuscitation. Resuscitation 2015;92:70-6. [Crossref] [PubMed]
- Shin TG, Jo IJ, Sim MS, et al. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol 2013;168:3424-30. [Crossref] [PubMed]
- Hajbaghery MA, Mousavi G, Akbari H. Factors influencing survival after in-hospital cardiopulmonary resuscitation. Resuscitation 2005;66:317-21. [Crossref] [PubMed]
- Hazinski MF, Nolan JP, Billi JE, et al. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122:S250-75. [Crossref] [PubMed]
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics—2016 Update—A Report From the American Heart Association. Circulation 2015;CIR.0000000000000350.
- Highlights of the 2015 AHA Guidelines Update for CPR & ECC. Available online: http://eccguidelines.heart.org/wp-content/uploads/2015/10/2015-AHA-Guidelines-Highlights-English.pdf
- Rosenthal R, Jacobson L. Pygmalion in the classroom. Urban Rev 1968;3:16-20. [Crossref]


