Extracellular vesicles: emerging mediators of intercellular communication and tumor angiogenesis
Rapidly expanding solid tumors demand large quantities of nutrients and oxygen. Growing tumors exploit pre-existing vessels and/or develop new vessels (vascularization) to obtain these nutrients. Vascularization is classified into two main processes, vasculogenesis and angiogenesis. Vasculogenesis is the formation of primitive blood vessels by endothelial progenitors, and angiogenesis encompasses the subsequent remodeling processes, including growth and migration of endothelial cells, sprouting, and stabilization of these sprouts by mural cells (1,2). Tumor cells utilize these processes to satisfy their needs and grow (tumor angiogenesis), especially under hypoxic conditions. One of the pro-angiogenic mechanisms exploited by hypoxic cancers is hypoxia-inducible transcriptional factor (HIF)-mediated signaling. Hypoxia leads to stabilization and nuclear translocation of HIF-1α, and subsequently increases transcription of pro-angiogenic genes, including vascular endothelial growth factor (VEGF) (3). Overexpression of HIF-1α has been reported in various solid tumors including brain, bladder, breast, colorectal, ovarian, pancreatic, and prostate cancers (4,5), and increased vascularity is a hallmark of poor prognosis.
Recent studies have offered new insights into the significant role of extracellular vesicles (EVs) in tumor angiogenesis. EVs are nanometer-sized membranous vesicles that carry genetic information including proteins, mRNAs, and microRNAs. EVs were previously thought to be waste materials; however, recent accumulating evidence has revealed that almost all cell types secrete and use EVs for horizontal exchange of cargo, that is, primitive intercellular communication. Cancer cells in particular are known to secrete large amounts of EVs to expand their niche. A recent article published in Oncology Research by Huang and colleagues demonstrated that HIF-1α is overexpressed in hypoxic colorectal cancer (CRC) cells, which increased Wnt4 secretion via EVs, activated Wnt/β-catenin signaling in recipient endothelial cells, and consequently promoted angiogenesis and tumor growth (6). This evidence has highlighted the importance of EVs as a tool for intercellular communication in rapidly expanding tumors. However, as EV biology is still a developing research field, several issues are currently the subject of intensive discussion.
How is cargo sorted and loaded into EVs?
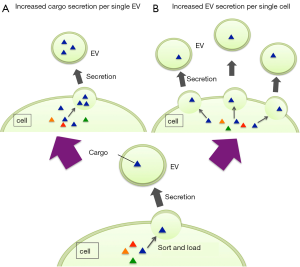
It remains unknown why EVs from hypoxic cancer cells have a stronger pro-angiogenic effect than normoxic cancer cells. Huang et al. showed that Wnt4 was enriched in EVs from hypoxic CRC cells compared with EVs from normoxic CRC cells. As shown in Figure 1A, it was unclear whether this was due to an increase in the quantity of specific cargo (in their study, Wnt4) loaded into single EVs. The standardized methods for EV isolation and quantification remain controversial (7). Furthermore, it remains unclear how cargoes are sorted and loaded into EVs. No specific molecule has been identified that can be used as an internal control for the quantity of EV contents. To date, researchers have managed to estimate relative quantities using various methods, including nanoparticle tracking analysis (NTA) to estimate the number of EVs per mL (medium) or per cell, and division of a specific cargo by the total quantity of EV proteins or EV RNAs to estimate the quantity of a specific cargo per EV (8-10). However, although these relative quantifications are acceptable for use in single studies, they cannot be used to conduct meta-analysis between independent studies. To promote further understanding of EV biology and the clinical significance of EVs, many challenges in the evaluation of EV contents remain.
Regulation of EV secretion
Again, why do EVs from hypoxic cancer cells have such a strong pro-angiogenic effect? As shown in Figure 1B, it might be due to an increase in the quantity of EVs secreted by single cells. However, it is possible that, although cargo quantity differs between EVs in (A) and (B), the total amount of cargo secreted per cell is the same. There is no method to distinguish them. It is also unknown which one we observe as “an increased secretion of cargo”. The mechanism of EV secretion is currently being intensively investigated, and the full picture is gradually being revealed.
Anti-angiogenic therapy has been studied as a powerful tool to prevent cancer progression by reducing the supply of nutrients and oxygen. The first anti-angiogenic molecular targeting agent, bevacizumab, which is an anti-VEGF-A monoclonal antibody, is now included in various chemotherapy regimens. There is a possibility that anti-EV secretion therapy will be a new strategy to starve tumors, by cutting off intercellular communication between cancer cells and stromal cells. Liquid biopsy for EVs is also considered to be a promising non-invasive method for cancer diagnosis and monitoring. Although many researchers tend to concentrate on the clinical utility of EV contents, basic knowledge of EV biology remains limited. I hope that furthering our understanding of EV biology will reveal the complex pathways of communication between the human body and tumors and contribute to the development of new cancer therapies.
Acknowledgements
Funding: This work was supported by JSPS KAKENHI [grant number 26870243].
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Carmeliet P. Angiogenesis in health and disease. Nat Med 2003;9:653-60. [Crossref] [PubMed]
- Coultas L, Chawengsaksophak K, Rossant J. Endothelial cells and VEGF in vascular development. Nature 2005;438:937-45. [Crossref] [PubMed]
- Shweiki D, Itin A, Soffer D, et al. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 1992;359:843-5. [Crossref] [PubMed]
- Zhong H, De Marzo AM, Laughner E, et al. Overexpression of hypoxia-inducible factor 1alpha in common human cancers and their metastases. Cancer Res 1999;59:5830-5. [PubMed]
- Talks KL, Turley H, Gatter KC, et al. The expression and distribution of the hypoxia-inducible factors HIF-1alpha and HIF-2alpha in normal human tissues, cancers, and tumor-associated macrophages. Am J Pathol 2000;157:411-21. [Crossref] [PubMed]
- Huang Z, Feng Y. Exosomes derived from hypoxic colorectal cancer cells promotes angiogenesis through Wnt4 induced β-catenin signaling in endothelial cells. Oncol Res 2016. [Epub ahead of print]. [PubMed]
- Witwer KW, Buzás EI, Bemis LT, et al. Standardization of sample collection, isolation and analysis methods in extracellular vesicle research. J Extracell Vesicles 2013.2. [PubMed]
- Yamada N, Kuranaga Y, Kumazaki M, et al. Colorectal cancer cell-derived extracellular vesicles induce phenotypic alteration of T cells into tumor-growth supporting cells with transforming growth factor-β1-mediated suppression. Oncotarget 2016;7:27033-43. [PubMed]
- Hoshino A, Costa-Silva B, Shen TL, et al. Tumour exosome integrins determine organotropic metastasis. Nature 2015;527:329-35. [Crossref] [PubMed]
- Boelens MC, Wu TJ, Nabet BY, et al. Exosome transfer from stromal to breast cancer cells regulates therapy resistance pathways. Cell 2014;159:499-513. [Crossref] [PubMed]


