A systematic review of combinatorial treatment with warming and invigorating drugs and levothyroxine for hypothyroidism caused by Hashimoto disease
Introduction
Hashimoto thyroiditis (HT), also known as chronic lymphocytic thyroiditis, is an autoimmune disease that was first described in 1912 by a Japanese scholar named Hashimoto (1). The disease is characterized by a diffuse goiter, lymphocytic infiltration, and thyroid autoantibodies. Although approximately 3–4% of Americans are known to suffer from HT (2), epidemiological data on HT in China are lacking. Females are 8–9 times more prone to HT than males, and individuals between 30–50 years of age are at high risk for HT. As individuals age, they become more prone to HT (1).
HT can be divided into three phases. Initially, a patient has normal thyroid function with transient hyperthyroidism. Then, as a result of the irreversible destruction of thyroid follicular cells, subclinical and clinical hypothyroidism arises gradually. Hypothyroidism is characterized by low metabolism and its corresponding symptoms, including fatigue, a low body temperature, a lag in response time, memory loss, unresponsiveness, irregular menstruation, mucosal edema, and may lead to further complications, such as osteoporosis, anemia, and hyperlipidemia. Hypothyroidism has been linked to cardiovascular diseases, including atrial fibrillation, coronary heart disease, pericardial effusion, and diverse nonspecific electrocardiogram (ECG) abnormalities (3). In short, patients suffering from hypothyroidism caused by HT should be diagnosed and treated early to prevent complications, and follow-ups are recommended even when thyroid function is normal. Patients with hypothyroidism are typically treated with levothyroxine as a thyroid hormone replacement to ensure that thyroid function remains within a normal range and to relieve clinical symptoms, but the efficacy of levothyroxine to reduce thyroid antibodies and goiter remains uncertain. Surgery is an option for patients with obvious goiters and for whom medication was not efficacious, but permanent hypothyroidism is common after surgery. Currently, modern medical treatments for HT have limitations. By combining modern medicine and traditional Chinese medicine (TCM), we may be able to achieve better HT therapies with fewer side effects.
According to TCM, HT is classified as a “wart disease”, whereas the resulting hypothyroidism is classified as a “wart disease”, a “consumptive disease”, or an “edema”. Previous studies have suggested that hypothyroidism is a result of deficiencies in Qi and Yang, thus, warming and invigorating drugs may be therapeutic and are described in the section on Shao yin disease in the text “Synopsis of Prescriptions of the Golden Chamber” (4). Recent studies have evaluated the efficacy of combining warming and invigorating drugs with levothyroxine to treat hypothyroidism caused by HT (5,6), however, the studies were inconclusive due to problems, such as small sample sizes and incorrect random allocations. This review aims to evaluate the previous studies according to evidence-based medicine to determine the validity and safety of combining warming and invigorating drugs with levothyroxine to treat hypothyroidism caused by HT.
Methods
Database and search strategies
We searched the Cochrane Library, Index Medicus, the Chinese Biomedical Literature Database, the China National Knowledge Infrastructure, and the Wanfang Data databases for randomized clinical trials (RCTs). “Hashimoto disease”, “medicine, Chinese traditional” and “thyroxine” were the medical subject headings (MESH) words, relevant entry words, and free words used to carry out the comprehensive search. To avoid bias, we did not limit the date of publication in our searches. Manual searches and other retrieval methods were also carried out.
Inclusion criteria
- Study type: randomized controlled trials.
- Participants: HT patients with hypothyroidism or subclinical hypothyroidism complications, but without other serious complications. HT was diagnosed according to “China’s Guidelines for the Diagnosis and Treatment of Thyroid Diseases” (1) or according to the Morita Mu standard (7) set by the Japanese Ministry of Health and Welfare. Hypothyroidism and subclinical hypothyroidism were diagnosed according to “China’s Guidelines for the Diagnosis and Treatment of Thyroid Diseases” (1,8).
- Interventions: warming and invigorating drugs were provided in a variety of forms, such as decoction, granules, and drugs with a Chinese patent.
- Comparison: levothyroxine.
Outcomes: free triiodothyronine (FT3), free thyroxine (FT4), thyroid stimulating hormone (TSH), thyroid autoantibodies, goiter reduction, changes in clinical symptoms, effects on TCM syndromes, total therapeutic effect, recurrence rate, and adverse reactions. Because FT3 and FT4 can be measured without thyroxine binding globulin (TBG), FT3 and FT4 can directly reflect thyroid function. TSH is secreted by the pituitary and stimulates secretion of thyroid hormone. TSH is regulated by the hypothalamus-pituitary-thyroid axis. Thyroid peroxidase antibody (TPOAb) and thyroglobulin antibody (TGAb) are two thyroid autoantibodies that are involved in HT diagnosis and prognosis. Goiter is a common symptom of HT, and it is assessed for by palpation or by color Doppler ultrasound. Changes in clinical symptoms are assessed using rating scales that compare individual symptom scores with total TCM syndrome scores. Effect on TCM syndromes refers to the reductions in TCM syndrome scores. Total therapeutic effect includes symptoms, signs, and laboratory examination. Recurrence rate refers to the proportion of disease recurrence after a long follow-up period. Adverse reactions include symptoms of discomfort, as well as abnormal liver function, kidney function, and ECG results.
Exclusion criteria
- Patients with thyroid nodules or thyroid cancer.
- Patients with hypothyroidism as a result of thyroid surgery or iodine therapy for hyperthyroidism.
- Children, pregnant women, and individuals with severe diseases involving the heart, brain, kidney, or other organ systems.
- Patients who have used other intervention measures, such as acupuncture, moxibustion, external application and iontophoresis of Chinese medicines.
- Patients in the control group who have used other treatments in addition to levothyroxine.
Literature selection and data collection
We selected literature according to our inclusion and exclusion criteria. We carefully read the relevant chapters in the Cochrane Handbook (9) and then created our data collection form according to evidence-base medicine theory. We extracted four types of information from the literature: basic information, verification of study eligibility, study characteristics, and methodological quality (risk of bias). Two reviewers collected data independently, and a third reviewer (Bo Li) reviewed the data and made the final decision when the two independent reviewers disagreed. Finally, we gathered and input data into an Excel form for statistical analyses.
Quality assessment for studies
We assessed the methodology quality of each of the included studies using a modified Jadad scale (10), which included four aspects: “randomization”, “allocation concealment”, “blinding”, “lost to follow-up/drop out”. Studies that scored 1 to 3 were considered low quality and studies that scored 4 to 7 were considered high quality.
Statistical analysis
RevMan 5.3 software provided by Cochrane Collaboration was used to analyze the data. Dichotomous data were expressed as relative risk (RR) and continuous outcomes were expressed as weighted mean difference (WMD) or standard mean difference (SMD) with 95% confidence intervals (CI). Heterogeneity was evaluated using the I2 test. The fixed-effect model was used for analysis if the heterogeneity was not significant, and the random-effect model was used for analysis if the heterogeneity was significant. Sensitivity analysis was performed to verify the stability of the results. Intention-to-treat analysis (ITT) and per-protocol (PP) analysis were used to analyze the dichotomous data of participants lost to follow-up.
Results
Search results
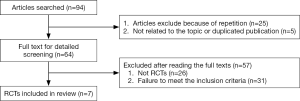
A total of 94 articles were retrieved, but 87 of these articles were excluded after review. A flow diagram of the article selection process is shown in Figure 1.
Characteristics of the included RCTs
Our search identified 7 eligible trials that were conducted in China, contained 472 participants with 241 participants in the experimental group and 231 participants in the control group. The characteristics of the included studies are shown in Table 1.

Full table
Methodology quality of the included trials
Methodology quality of the included studies was assessed using a modified Jadad scale. A score of 4–7 points indicated a high-quality study and a score of 1–3 points indicated a low-quality study. Of the seven included studies, four received scores of 1 point, two received scores of 2 points, and one received a score of 2.5 points (Table 2).
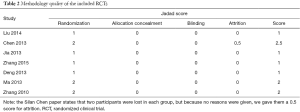
Full table
Meta-analysis
FT4
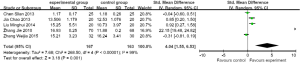
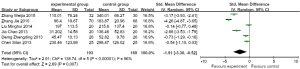
FT4 was measured in five of the studies (11-14,17). Because the different studies measured FT4 using different units, we used SMD to describe the effects on FT4 levels and calculated 95% CIs. Pooled data revealed differences in FT4 levels [SMD =4.04 (1.55, 6.53), P=0.001 (<0.05); heterogeneity: Chi2 =268.50, P<0.00001, I2 =99%] (Figure 2).
The forest plots and full texts of the RCTs indicated that the Jie Zhang, Silan Chen, and Weijia Zhang trials may be the source of the heterogeneity. Sensitivity analysis showed an unstable quantitative analysis. The FT4 level was higher in the experimental group than in the control group, thus warming and invigorating drugs in combination with levothyroxine may increase FT4 levels in patients with hypothyroidism caused by HT. However, this result was not stable, perhaps because of the small sample size and the heterogeneity between studies.
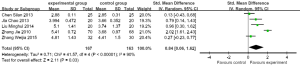
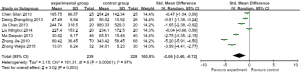
FT3
FT3 was measured in five of the studies (11-14,17). Because the different studies measured FT3 using different units, we used SMD to describe the effects on FT3 levels and calculated 95% CIs. Pooled data revealed differences in FT3 levels [SMD =0.84 (0.06, 1.62), P=0.03 (<0.05); heterogeneity: Chi2 =41.57, P<0.00001, I2 =90%] (Figure 3).
The forest plots and full texts of the RCTs indicated that the Jie Zhang, Silan Chen, and Weijia Zhang trials may be the source of heterogeneity. Sensitivity analysis showed a stable meta-analysis. The FT3 levels in the experimental group were higher than in the control group suggesting that the combination of warming and invigorating drugs and levothyroxine may increase FT3 levels in patients with hypothyroidism caused by HT. In addition, this result was stable.
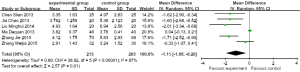
TSH
TSH was measured in six of the studies (11-14,16,17). Because the units of measurement used were the same in all of the studies, we used WMD to describe the effects on TSH levels and calculated 95% CIs. Pooled data showed differences in TSH levels [WMD =−1.11 (−1.95, −0.26), P=0.01 (<0.05); heterogeneity: Chi2 =38.92, P<0.00001, I2 =87%] (Figure 4).
Forest plots and full texts of the RCTs indicated that the Weijia Zhang and Dequan Ma trials may be the source of the heterogeneity. Sensitivity analysis showed a stable quantitative analysis. The TSH levels in the experimental group were lower than in the control group suggesting that the combination of warming and invigorating drugs and levothyroxine may reduce TSH levels in patients with hypothyroidism caused by HT. In addition, this result was stable.
TPOAb
TPOAb was measured in six of the studies (11-15,17). Because different units of measurement were used in the different studies, we used SMD to describe the effects on TPOAb levels and calculated 95% CIs. Pooled data showed differences in TPOAb levels [SMD =−1.91 (−3.30, −0.52), P=0.007 (<0.05); heterogeneity: Chi2 =138.74, P<0.00001, I2 =96%] (Figure 5).
The forest plots and full texts of the RCTS indicated that the Jie Zhang and Weijia Zhang trials and the different measurement units used may be the source of the heterogeneity. Sensitivity analysis revealed a stable quantitative analysis. The TPOAb levels in the experimental group were lower than in the control group suggesting that the combination of warming and invigorating drugs and levothyroxine reduce TPOAb levels in patients with hypothyroidism caused by HT. In addition, this result was stable.
TGAb
TGAb was measured in all seven of the studies (11-17). Because different units of measurement were used in different studies, we used SMD to describe the effects on TGAb levels and calculated 95% CIs. Pooled data showed differences [SMD =−2.06 (−3.40, −0.72, P=0.03); heterogeneity: Chi2 =181.31, P<0.00001, I2 =97%] (Figure 6).
The forest plots and full texts of the RCTs indicated that the Jie Zhang and Weijia Zhang trials may be the source of the heterogeneity. Sensitivity analysis revealed a stable quantitative analysis. The TGAb levels in the experimental group were lower than in the control group suggesting that the combination of warming and invigorating drugs and levothyroxine reduced TGAb levels in patients with hypothyroidism caused by HT. This result was stable.
Goiter
The Chao Jia study (13) was the only one that gave detailed descriptions of the goiter classification before and after treatment. However, the rank sum test indicated no significant difference between the experimental and control groups after treatment. Treatment with warming and invigorating drugs combined with levothyroxine was as ineffective in reducing the goiter as levothyroxine alone.
TCM syndrome score
TCM syndrome scores were analyzed in three of the studies (12,13,17). The Silan Chen study described five symptoms, including thyroid oppression, fatigue, chills, loose stool, and irascibility, and with the exception of irascibility, significant differences in individual TCM syndrome scores were observed between the experimental and control groups after treatment. The Chao Jia study described several symptoms, including fatigue, laziness to speak, edema, and forgetfulness, and the experimental group had fewer of these symptoms than the control group. The Jie Zhang study described fatigue, soreness and weakness at the waist and knees, laziness to speak, and decreased appetite, and the TCM syndrome scores were lower after treatment with a combination of warming and invigorating drugs and levothyroxine than with levothyroxine alone. The Jie Zhang and Chao Jia studies also performed statistical analyses on total TCM syndrome scores, but we did not pool the data because different symptoms were evaluated in the different trials.
Effect on TCM syndrome
The effects on TCM syndromes were evaluated in three of the studies (12,13,17). We transformed the ordinal data used to describe the TCM effects into binary data, including efficacy and inefficacy. We used RR to describe the effects and calculated 95% CIs. Pooled data revealed no significant differences [RR =1.49 (0.99, 2.23), P=0.06; heterogeneity: Chi2 =11.90, P=0.003, I2 = 83%] (Figure 7).
The forest plots and full texts of the RCTs indicated that the study by Chao Jia may be the source of the heterogeneity. Data were pooled again after excluding the Chao Jia study and significant differences were found. Because the Silan Chen trial described attrition, we carried out ITT analysis and no significant differences were found. Warming and invigorating drugs combined with levothyroxine had a similar effect on TCM syndromes as levothyroxine alone.
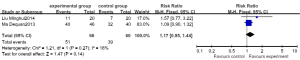
Total therapeutic effect
The total therapeutic effect was analyzed in three of the studies (11,14,16), but the data in the Weijia Zhang study is too inaccurate to be pooled. In the Dequan Ma study, the total effective rate in both groups was 100%. We transformed the ordinal data into binary data and used RR to describe the effective rate. Pooled data revealed no significant differences [RR =1.17 (0.95, 1.44), P=0.14; heterogeneity: Chi2 =1.21, P=0.27, I2 =18%] (Figure 8).
Recurrence rate
The Dequan Ma article (16) was the only study that described recurrence rate after following up for half a year, but the data is too inaccurate for further statistical analysis.
Adverse reactions
The Minghui Liu (11), Jie Zhang (17) and Chao Jia (13) studies addressed adverse reactions. Routine blood, urine, stool, liver function, kidney function, and ECG tests were normal during treatment and none of the participants reported adverse reactions.
Discussion
Current treatment of hypothyroidism caused by HT
Currently, there is no treatment that targets the pathology of HT. For the hypothyroidism stage of HT, treatment with levothyroxine is a recognized therapy. Although levothyroxine recovers thyroid function, the evidence that it reduces antibody levels and goiter is insufficient. Hypothyroidism caused by HT is classified as “wart disease”, “consumptive disease”, or “edema” in TCM and is usually diagnosed as a Qi and Yang deficiency. Thus, warming and invigorating drugs combined with levothyroxine usually achieves satisfactory therapeutic effects.
Meta-analysis results
FT4
We pooled FT4 data from five original trials and found a significant difference between the experimental and control groups. This suggests that the combination of warming and invigorating drugs and levothyroxine may increase FT4 levels more than levothyroxine alone. However, this result was not stable due to several factors, such as a small sample size, heterogeneity caused by the use of different units of measurement, and application of the random-effect model, thus the conclusion needs further confirmation. Inconsistent measurements are inconvenient and hinder clinical practice and scientific research. Different medical institutions adopt different clinical test methods and reagents leading to differences in units and references. Hence, laboratory results of the same item from different hospitals are incomparable, which makes evaluation of clinical curative effects inconvenient, wasteful, and aggravates the economic burden for patients. In scientific research, different research methods use different test units. As a result, researchers must standardize the original data using statistical methods in order to pool the data. Inescapably, bias appears during this process and some of the credibility of the results will be lost. We suggest that the Chinese Society of Endocrinology formulate uniform test methods to ensure consistency in units and references across the country to enhance academic communication across different regions.
FT3
We pooled FT3 data from five original trials and obtained a stable result showing a significant difference between the experimental and control groups. We found that the combination of warming and invigorating drugs and levothyroxine increased FT3 levels more than levothyroxine alone. Although FT3 is not the first choice test to diagnose hypothyroidism, FT3 is significant because it is the biologically active form of thyroxine in the human body and 80% of T3 arises from the conversion of T4.
TSH
We pooled TSH from six original trials and obtained a stable result showing a significant difference between the experimental and control groups. We found that the combination of warming and invigorating drugs and levothyroxine reduced TSH more than levothyroxine alone. In patients suffering from hypothyroidism caused by HT, thyroid follicular cells are damaged by inflammation leading to low levels of thyroxine production. More TSH is then generated via the negative feedback mechanisms of the hypothalamus-pituitary-thyroid axis, thus TSH levels can reflect curative effects on hypothyroidism.
TPOAb
We pooled TPOAb data from six original trials and obtained a stable result revealing a significant difference between the experimental and control groups. We found that the combination of warming and invigorating drugs and levothyroxine reduced TPOAb levels more than levothyroxine alone. Studies (18-20) have shown that TPOAb is associated with the occurrence of HT and hypothyroidism and that a higher TPOAb level leads to more severe autoimmune damage. Therefore, TPOAb is an important indicator for the prognosis of hypothyroidism caused by HT.
TGAb
All of the seven RCTs measured TGAb, and we pooled the data by meta-analysis and obtained a stable result revealing a significant difference between the experimental and control groups. We found that the combination of warming and invigorating drugs and levothyroxine reduced TGAb more than levothyroxine alone. A previous study (21) showed that TGAb and TPOAb are important pathogenic factors and indicators of HT, thus determining TGAb levels is important to evaluate HT treatment efficacy.
Goiter
There was only one original study that described and classified goiter before and after treatment, and the rank sum test showed no significant difference between the experimental and the control groups suggesting that the combination of warming and invigorating drugs and levothyroxine was as ineffective as levothyroxine alone. Although the pathology of HT remains unclear, goiter may be associated with autoimmunity and autoregulation of thyroxine, and it is often very difficult to alleviate goiter in a short period of time. As a primary characteristic of HT, goiter should be considered an important index to evaluate efficacy of treatment. Because only one study described goiter, more evidence is necessary to confirm whether the combination of warming and invigorating drugs and levothyroxine reduces goiter more than levothyroxine alone. Further, there is no unified standard to describe the degree of goiter, for example, goiter is divided into light, medium and heavy categories in “Guiding Principles of Clinical Research on New Drugs of Traditional Chinese Medicine” (22) and into categories I, II, and III by palpation in “China’s Guidelines for the Diagnosis and Treatment of Thyroid Diseases” (23). Therefore, we suggest that the Chinese Society of Endocrinology formulate uniform test methods and standards to evaluate goiter.
TCM syndromes score
Three of the RCTs described individual TCM syndromes scores and two of the RCTs performed statistical analyses on the total TCM syndromes scores. The individual studies showed that the combination of warming and invigorating drugs and levothyroxine relieved symptoms more than levothyroxine alone, but, we did not pool or perform meta-analysis on the outcomes because different TCM symptoms were evaluated in the different studies. Because TCM is a type of empirical medicine with poor reproducibility, we should reinforce normalization and standardization of the methods to diagnose TCM syndromes, and RCTs of high quality are necessary to evaluate TCM syndromes.
Effects on TCM syndromes
Three of the studies calculated and analyzed the effects on TCM syndromes. We pooled the outcomes and the meta-analysis showed no statistically significant differences between the experimental and control groups. However, according to the Cochrane Handbook (9), when the 95% CI is larger than 1 and the horizontal line falls on the right side of the invalid line, a higher effective rate in the experimental group than in the control group should be considered. Because the 95% CI is 0.99, which is very close to 1, and because the majority (95%) of the horizontal line fell on the right side of invalid line, the data lean towards statistical significance. We speculate that a significant result would have been obtained if the sample size were larger. In addition, forest plots indicated that one of the studies contributed to heterogeneity. When that study was excluded by PP or ITT analyses, statistical differences were revealed, thus the combination of warming and invigorating drugs and levothyroxine may improve TCM syndromes resulting from hypothyroidism caused by HT more than levothyroxine alone.
Total therapeutic effects
Two of the studies performed statistical analyses on total therapeutic effects. The outcomes were pooled and meta-analysis showed no significant difference between the experimental and control groups, which may be the result of a small sample size. We suggest that the China Society of Endocrinology establish unified efficacy standards to evaluate HT, and we suggest that scientific researchers should report total therapeutic effects.
Recurrence rate
Only one of the RCTs described the recurrence rate after a half-year follow-up visit, however, we did not analyze the data further because of inaccuracies in the data. Hypothyroidism is a consequence of modern medicine-based HT treatment, and patients with hypothyroidism are typically on medication permanently, which may bring about mental pressures. As a result, follow-up visits are necessary even if thyroid function has recovered to a normal level. We suggest that more follow-up visits should occur during clinical trials on HT to better evaluate the efficacy and safety of drugs. If sufficient evidence reveals that TCM treatments can reduce the recurrence rate of hypothyroidism in HT patients, HT treatments will be expanded.
Adverse reactions
Three of the studies described adverse reactions. According to the original studies, no adverse reactions occurred in any of the participants. There are two sides to any medication; on one hand, medications cure diseases and recover the body to normal function, whereas on the other hand, medications damage the body. Therefore, safety should be equally as important as efficacy when evaluating medications. Chinese herbal medicines are typically safe and lead to few adverse reactions, however, nothing is absolute and adverse reactions arising from TCM should be given more attention in clinical practice and scientific research.
Open questions
There are several open questions and limitations in this systematic review. First, we only retrieved studies from English and Chinese databases, therefore, some studies may have been missed, which may have led to sampling bias. Second, because only seven RCTs were included, publication bias was inevitable. Third, the methodological qualities of the included studies were low, which may have led to selection bias, performance bias, and attrition bias. Lastly, clinical heterogeneity may be a result of the differences between the studies, such as differences in the severities of the disease cases and differences in the treatment dosages.
Conclusions
This systematic review pooled several indices of hypothyroidism caused by HT according to “China’s Guidelines for the Diagnosis and Treatment of Thyroid Disease” and correlation studies (1,8). The results showed that the combination of warming and invigorating drugs and levothyroxine increased FT3 and FT4 levels, and reduced TSH, TPOAb, and TGAb levels in patients with hypothyroidism cause by HT more than levothyroxine alone after treatments of 8 weeks or longer. With the exception of FT4, the results were stable. This conclusion is in accordance with Zixiao Wei and his clinical experiences with HT (3).
In conclusion, we cautiously recommend prescribing warming and invigorating drugs along with levothyroxine for the treatment of hypothyroidism caused by HT. However, high-quality evidence is needed to confirm these results. To guarantee evidence quality, a strict study design, which includes a large sample, an unbiased randomization method, full concealment, proper blinding, and appropriate statistical analyses, is vital. In addition, clinical curative effects of TCM, such as TCM syndromes, should be standardized and unified to reduce clinical heterogeneity and methodology heterogeneity. Finally, a strict registration system for clinical trials is required to remove reporting biases.
Acknowledgements
We are sincerely grateful to the Evidence-Based Clinical Club (EBC) for providing guidance and help with the systematic review process.
Funding: Supported by the National Natural Science Foundation of China (No. 81303151), and Beijing NOVA Program (No. xxjh2015A093 and No. Z1511000003150125).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Editorial committee of China's guidelines for the diagnosis and treatment of thyroid diseases. China's guidelines for the diagnosis and treatment of thyroid diseases. Beijing: Chinese Society of Endocrinology, 2008:50-4.
- Goldman L, Ausiello D, Wang X. editors. Cecil Textbook of Medicine. Xi’an: World Book Publishing Xi’an Co. Ltd., 2009:2148.
- Wang XL, Wu SL. Hypothyroidism and cardiovascular diseases. Chinese Journal of Cardiovascular Research 2006;9:670-2.
- Wei ZX. editor. Experience is the traditional Chinese medicine. Beijing: People's Medical Publishing House, 2010:164-6.
- Chen QK, Zheng SX, Liu J. Application of ER Xian Tang and QI Hai Xiao Ying Tang for treatment of chronic lymphocytic thyroiditis complicated with hypothyroidism. Laboratory Medicine and Clinic 2014;8:1023-4.
- Jiang LL, Wu J, Zhang DX, et al. Application of WEN Yang Xiao Ying Tang for treatment of chronic lymphocytic thyroiditis complicated with hypothyroidism. Modern Journal of Integrated Traditional Chinese and Western Medicine 2011;6:705-6.
- Gao XW, Li JL. editors. Thyroid diseases. Beijing: People's Medical Publishing House, 1999:190-3.
- Editorial committee of China's guidelines for the diagnosis and treatment of thyroid diseases. China's guidelines for the diagnosis and treatment of thyroid diseases. Beijing: Chinese Society of Endocrinology, 2008:31-40.
- Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available online: www.cochrane-handbook.org
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [Crossref] [PubMed]
- Liu MH, Zhang CF, Ma J. Clinical observation on effect of YI Yuan Ying Xiao Tang on hypothyroidism caused by Hashimoto Disease. Jiangxi Journal of Traditional Chinese Medicine 2014;8:39-41.
- Chen SL, Li GQ, Gao DM. Clinical studies of reinforcing kidney and strengthening spleen and soothing liver prescription on treating Hashimoto’s thyroiditis. Global Traditional Chinese Medicine 2013;4:245-9.
- Jia C. Clinical observation and research of Fuzhengsanying Decoction curing hypothyroidism causing of Hashimoto’s thyroiditis. Shandong University of Traditional Chinese Medicine, 2013.
- Zhang WJ, Zhang ZX, Cheng W, et al. Clinical observation on Gubenxiaosan Decoction curing 62 cases of hypothyroidism causing of Hashimoto’s thyroiditis. Journal of Clinical Medicine in Practice 2015;11:156-8.
- Deng ZD. Effect of WenYanSanJie method on Hashimoto’s thyroiditis with hypothyroidism. Health 2013;4:428,286.
- Ma DQ. Clinical observation on the therapeutic effect of integrative medicine therapy on Hashimoto thyroiditis complicated with subclinical hypothyroidism. Acta Chinese Medicine 2013;28:1382-3.
- Zhang J. Effect of Buyuan Capsule and Euthyrox for Hashimoto’s hypothyroidism-a clinical observation on 70 cases. Journal of Traditional Chinese Medicine 2010;8:701-3.
- Shang DH. Measurement and analysis of TPOAb in 121 patients suffering from hyperthyroidism. Fujian Medical Journal 2008;30:97-8.
- Hu X, Bin MH. Analysis on TPOAb level of different thyroid function state in thyroid diseases. Guangxi Medical Journal 2008;30:1701-2.
- Guo SH, Zhao SJ, Wang WY. Meaning of detection of TGAb and TPOAb in autoimmune thyroid diseases. Clinical Medicine 2007;27:81-2.
- Wang X, Zhang HY. The clinical application of quantitative analysis of thyroid autoantibodies in serum. Chinese Journal of Laboratory Diagnosis 2010;8:1249-51.
- Zheng XY. editor. Guiding principles of clinical research on new drugs of traditional Chinese medicine (trial). Beijing: China Medical Science Press, 2002:226-30.
- Editorial committee of China's guidelines for the diagnosis and treatment of thyroid diseases. China's guidelines for the diagnosis and treatment of thyroid diseases. Beijing: Chinese Society of Endocrinology, 2008:42-5.