A rare case of a blood clot masquerading as a retained surgical drain
Introduction
Surgical drains are routinely used in various forms of surgery to reduce post-operative fluid collections. Removal of these surgical drains is an easily performed bedside procedure. A retained surgical drain during removal is a rare but potentially serious complication which can cause significant distress in both the patient and the surgeon.
There is a paucity of literature on retained surgical drains and their effects in orthopaedic surgery (1,2). Whilst there is a theoretical risk of infection, fibrosis and pain as a result of these retained drains, some reports have shown that there are minimal long term sequelae with retained drains (3). Nonetheless, in view of these potential clinical complications as well as medico-legal considerations, surgeons should minimize such occurrences and be aware of how to confirm the presence of a retained drain segment. We report a case of a blood clot masquerading as a retained surgical drain in a patient who underwent drainage for left gluteal necrotizing fasciitis.
Case presentation
The patient is a 55-year-old Malay male with a known medical history of diabetes and chronic renal impairment. He presented to our institution in May 2016 for left thigh and gluteal necrotizing fasciitis. The patient was started on ceftazidime and underwent an initial debridement with negative pressure therapy dressings applied. The patient underwent a further four debridements. On the 5th debridement, the wound was deemed sufficiently clean and the wound was closed. Two Redivac drains (size 12 mm) were inserted, with one inserted into the gluteal region and the other into the proximal thigh. On post-operative day 2, the drain in the gluteal region was no longer draining and was removed at the bedside. There were no difficulties in drain removal and the tip of the drain was noted to be intact. The drain from the proximal thigh was removed 3 days later and the removal was uneventful.
Seven days later, it was noted that there was serous discharge from the mid portion of the wound. A magnetic resonance imaging (MRI) scan of the left gluteus and thigh was performed and it revealed a large collection in the gluteal region. Incidentally, it was noted that there was a tubular structure resembling that of a drain segment in the gluteal region (Figure 1). The patient was informed of the need to undergo operative evacuation of the collection and the retained drain segment was to be removed concurrently.
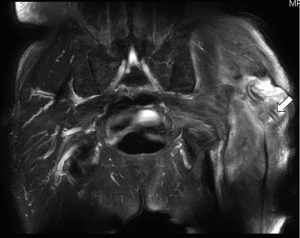
Intra-operatively, the collection was noted to be a large hematoma and was evacuated. However, the drain segment seen on MRI was not found and instead, a tubular blood clot of similar caliber and length as measured on the MRI was found residing in the gluteal region (Figure 2). An intra-operative radiograph performed revealed no retained drain segment in the gluteal region. The patient’s wounds healed uneventfully thereafter.

Discussion
Retained surgical drains are rare events but may result in anxiety for both patient and surgeon. With few reports in the existing literature of the long-term effects of a retained drain, coupled with the rising threat of medical litigation, surgeons may advocate surgical exploration and removal. These re-operations place the patient at additional anaesthetic and surgical risks. As such, it is critical to be certain of a retained surgical drain prior to advocating surgical removal.
There are several advocated methods to prevent retained surgical drains. Intra-operatively, surgeons should be cautious during wound closure so as not to stitch the drain segment within soft tissue. Surgeons should also ensure that the angle at which the drain exits the skin should not be too acute. These measures allow for drain removal to be smooth and without undue resistance. The length of the in-situ drain should also be measured and documented so as to compare the drain segment upon removal. Upon removal, the drain tip should be inspected to ensure that no fracture of the drain tip has occurred. In our case, the drain removal was a smooth and painless procedure. The removed drain tip was also inspected, which revealed a complete drain segment. However, there was no comparison of the removed drain length with that of the length documented intra-operatively.
Plain radiographs should be performed in the setting of a retained drain segment. Silicon surgical drains are radio-opaque, designed to improve detection of surgical drain tube placement. Pre-operative radiographs will allow the surgeon not only to confirm the presence of a retained segment, but also provides information on the exact location. In our case, the magnetic resonance imaging performed revealed a large hematoma with a tubular like structure, thought to be a retained drain segment. This image was created by the tubular blood clot, likely to have been formed when the drain was in vivo. At this juncture, a pre-operative radiograph should have been performed to confirm the presence of a retained drain segment. Nonetheless, our patient required a surgical evacuation of the hematoma and thus there were no unnecessary anaesthetic or surgical risks to the patient.
Conclusions
Retained surgical drains are rare but potentially avoidable events. Surgeons should be certain of the presence of a retained surgical drain before advocating for surgical removal. When in doubt, plain radiography remains a useful modality for visualization of radio-opaque surgical drains.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Liu KS, Huang KC, Wong CH. A neglected retained penrose drain mimicking an amputation stump neuroma. J Trauma 2007;62:1051-2. [Crossref] [PubMed]
- Gheorghiu D, Cowan C, Teanby D. Retained surgical drain after total knee arthroplasty: an eight-year follow-up. JBJS Case Connect 2015;5:e63. [Crossref]
- Gausden EB, Sama AA, Taher F, et al. Long-term sequelae of patients with retained drains in spine surgery. J Spinal Disord Tech 2015;28:37-9. [Crossref] [PubMed]


