Fatty acid-binding proteins as diagnostic and prognostic markers in pneumonia
Pneumonia remains a potentially life threatening infection. The incidence of community acquired pneumonia (CAP) differs by region, season and the characteristics of the population under evaluation. A recent review on CAP among adults in Europe found the incidence ranged from 1.54 to 1.70 per 1,000 population, rising to as high as 14.0 cases per 1,000 person-years in those aged 65 years and over (1). Mortality for patients hospitalised with CAP ranges from 5.1–36.5%. The mortality is particularly high in critically ill patients with pneumonia who require admission to intensive care units (ICUs) and reported figure is as high as 57.3% (2).
The diagnosis and prognosis of pneumonia can be challenging. Clinical presentation typically involves a combination of fever, productive cough, dyspnoea, chest pain, associated with leucocytosis and the consolidation in the Chest-X-ray. However, CAP may present very differently in certain patient groups such as the elderly who tend to display very non-specific symptoms such as abdominal pain/discomfort, confusion or an altered level of consciousness. The cardinal symptoms such as fever, cough and signs such as leucocytosis may not be present in this age group (3). Further, parenchymal opacifications may not be present in chest radiographs in up to one fifth of patients with CAP (4).
This potential difficulty in diagnosis is coupled with a difficulty in prognosis. Due to the importance of predicting the severity of pneumonia and determining which patients require more intensive treatment, various risk scores have been developed. Commonly used scores include the CURB scoring system (CURB, CRB-65 and CURB-65) developed in the United Kingdom and Pneumonia Severity Index (PSI) in the United States. A recent meta-analysis evaluated the ability of PSI and the different risk scales in the CURB scoring system to predict mortality in pneumonia patients (5). No particular scale was found to be superior on all counts. CURB, CRB-65 and CURB-65 were found to be more specific and to have higher positive predictive value; they are able to correctly classify a larger proportion of the ‘high risk’ patients than PSI. Conversely, PSI was more sensitive with a lower false negative predictive value; it was best able to identify patients who did not have severe pneumonia and were at low risk of death. Despite the shortcomings of these risk scores, both remain clinically useful (5). However, both scores may benefit by being augmented or complemented by additional means of predicting outcomes in CAP patients.
In a recent issue of Medicine, Tsao and colleagues evaluated the effectiveness of urinary fatty acid-binding proteins (FABPs) as markers of severity and treatment response in critically ill patients with pneumonia (6). FABPs have been investigated as biomarkers for the prognosis and diagnosis of various severe medical conditions including myocardial infarction (7), pulmonary embolism (8) and heart failure (9). FABPs are a family of small (12–20 kDa) cytoplasmic proteins involved in the transportation and storage of lipids. They have various functions including the regulation of fatty-acid-responsive-gene expression, maintaining fatty acid levels in cell membranes, intracellular long-chain fatty acid transportation and modulating metabolic pathways involving lipids (10). While specific types of FABP are primarily expressed in certain types of tissue, they often have a varied tissue distribution (Table 1).
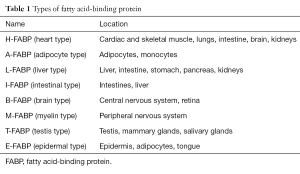
Full table
The study conducted by Tsao and colleagues consisted of a well-designed cross-sectional study of 62 patients, 50 of whom had pneumonia and 12 controls. Cases and controls were well-balanced in terms of population characteristics and subsequent analysis adjusted for a wide array of relevant confounders. Outcomes such as ‘clinical improvement’ were well defined and various inflammatory markers and procalcitonin were included for comparison. While urinary FABPs were not found to be associated with pneumonia when compared to non-infected patients, analysis was also stratified between pneumonia patients who did and did not have septic shock. Of the four FABPs assessed, multivariate analysis found elevated adipocyte-FABP to be independently associated with septic shock on day 1 of admission to ICU (P=0.026). In addition, comparison between patients who did and did not show improvement showed elevated adipocyte-FABP to be associated with those who did not show improvement at 7 days (P value =0.022). These findings suggest that urinary adipocyte-FABP may be useful in predicting the severity of CAP and in assessing response to treatment.
As the first study investigating the prognostic value of urinary FABPs in pneumonia, the findings of Tsao and colleagues carries an important new knowledge. While urinary FABPs are not likely to be useful in distinguishing between pneumonia and non-pneumonia patients, the findings of this study suggest that they may serve as useful prognostic indicators in those admitted with CAP, due to the association of elevated urinary adipocyte-FABP with respiratory sepsis. This raises the intriguing possibility that urinary FABPs may be sensitive marker to predict the severity of CAP in general. However, this was not assessed in Tsao; in fact for unclear reason Tsao and colleagues chose to exclude patients who had pneumonia for over 24 hours prior to admission to ICU. The addition of FABPs to established clinical risk scores such as CURB-65 and PSI to improve the predictive usefulness of these existing scores is potentially fruitful avenue for future research.
Previous studies investigating the efficacy of FABP’s in sepsis have focused on serum levels of FABPs as opposed to urinary levels. Elevated serum adipocyte-FABP has been found to predict mortality and insulin resistance in patients with sepsis (11). Furthermore, elevated serum heart type-FABP has been found to be associated with increased 28-day mortality (12) and organ dysfunction (13) in patients with sepsis. Future studies investigating the usefulness of FABP in pneumonia prognosis should therefore assess both serum and urinary levels as findings from previous studies have suggested both are potentially useful. In terms of sample population, larger scale studies with sufficient statistical power are also required to confirm these findings. While Tsao and colleagues assessed the ability of urinary-FABPs to predict septic shock, future studies would benefit from further exploring the association between elevated urinary-FABPs and sepsis by stratifying analysis between all three sub-types; sepsis, severe sepsis and septic shock. Finally, all four studies which have assessed the association between sepsis and FABPs to date have been conducted in Chinese patients. Whether or not the association between elevated FABPs and sepsis in patients from other ethnic backgrounds therefore warrants investigation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Torres A, Peetermans WE, Viegi G, et al. Risk factors for community-acquired pneumonia in adults in Europe: a literature review. Thorax 2013;68:1057-65. [Crossref] [PubMed]
- Fine MJ, Smith MA, Carson CA, et al. Prognosis and outcomes of patients with community-acquired pneumonia. A meta-analysis. JAMA 1996;275:134-41. [Crossref] [PubMed]
- Musher DM, Thorner AR. Community-acquired pneumonia. N Engl J Med 2014;371:1619-28. [Crossref] [PubMed]
- Hagaman JT, Rouan GW, Shipley RT, et al. Admission chest radiograph lacks sensitivity in the diagnosis of community-acquired pneumonia. Am J Med Sci 2009;337:236-40. [Crossref] [PubMed]
- Loke YK, Kwok CS, Niruban A, et al. Value of severity scales in predicting mortality from community-acquired pneumonia: systematic review and meta-analysis. Thorax 2010;65:884-90. [Crossref] [PubMed]
- Tsao TC, Tsai HC, Chang SC. Clinical Usefulness of Urinary Fatty Acid Binding Proteins in Assessing the Severity and Predicting Treatment Response of Pneumonia in Critically Ill Patients: A Cross-Sectional Study. Medicine (Baltimore) 2016;95:e3682. [Crossref] [PubMed]
- Carroll C, Al Khalaf M, Stevens JW, et al. Heart-type fatty acid binding protein as an early marker for myocardial infarction: systematic review and meta-analysis. Emerg Med J 2013;30:280-6. [Crossref] [PubMed]
- Ruan LB, He L, Zhao S, et al. Prognostic value of plasma heart-type fatty acid-binding protein in patients with acute pulmonary embolism: a meta-analysis. Chest 2014;146:1462-7. [Crossref] [PubMed]
- Arimoto T, Takeishi Y, Shiga R, et al. Prognostic value of elevated circulating heart-type fatty acid binding protein in patients with congestive heart failure. J Card Fail 2005;11:56-60. [Crossref] [PubMed]
- Storch J, Thumser AE. The fatty acid transport function of fatty acid-binding proteins. Biochim Biophys Acta 2000;1486:28-44. [Crossref] [PubMed]
- Huang CL, Wu YW, Hsieh AR, et al. Serum adipocyte fatty acid-binding protein levels in patients with critical illness are associated with insulin resistance and predict mortality. Crit Care 2013;17:R22. [Crossref] [PubMed]
- Zhang ZC, Dai HW, Yu YH, et al. Usefulness of heart-type fatty acid-binding protein in patients with severe sepsis. J Crit Care 2012;27:415.e13-8. [Crossref] [PubMed]
- Chen YX, Li CS. The prognostic and risk-stratified value of heart-type fatty acid-binding protein in septic patients in the emergency department. J Crit Care 2014;29:512-6. [Crossref] [PubMed]


