Hepatitis B virus infection and risk of coronary artery disease: a meta-analysis
Introduction
Coronary artery disease (CAD) raises health concerns as the major cause of sudden death in the United States. It affects more than 17.8 million American in 2010 (1). Risk factors of CAD include age, male sex, smoking, diabetes mellitus, hypercholesterolemia and hypertension (2). More recently, it has been demonstrated that chronic inflammatory state associated with chronic infection and chronic autoimmune disease, such as chronic hepatitis C virus (HCV) infection, rheumatoid arthritis and inflammatory myositis, could also be an independent risk factor for CAD (3-6).
Chronic hepatitis B virus (HBV) infection is one of the most common chronic infections affecting approximately 2.8 billion patients worldwide (7). In consideration of chronic inflammation, chronic HBV-infected patients might have a higher possibility of developing CAD. However, data on the relationship between HBV and CAD remains inconclusive as studies have yielded conflicting results (8-12). This systematic review and meta-analysis was conducted to summarize all available evidence to assess the risk of CAD among HBV-infected patients.
Methods
Search strategy
Published studies were retrieved independently by two authors (Karn Wijarnpreecha and Patompong Ungprasert) from MEDLINE and EMBASE database for available literatures up to June 2016. Electronic search strategy was performed by integrating the terms for “hepatitis B virus” in conjunction with the term “coronary artery disease”. Additional data is described in Table S1. Non-English publications were included. Further evaluation for potential relevant studies was performed manually on bibliography of selected searched articles.
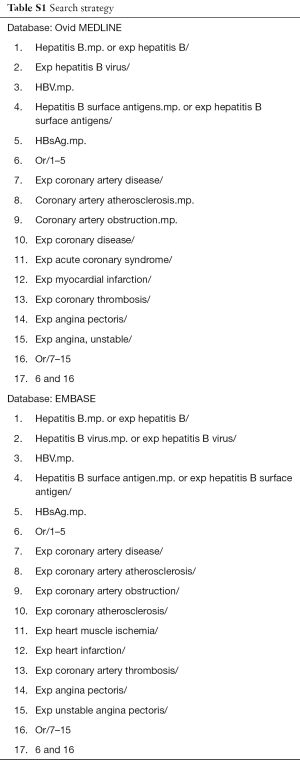
Full table
Inclusion criteria
We included studies that met the following inclusion criteria: (I) observational studies (case-control, cross-sectional or cohort studies) published as original articles to determine the risk of CAD among HBV-infected patients compared with subjects without HBV infection; (II) detailed odds ratio (OR), relative risk (RR), hazard ratio (HR) or standardized incidence ratio (SIR) with 95% confidence interval (CI) were given. If the ratios were not available, the study must provide adequate calculable raw data.
Retrieved studies were independently reviewed for their eligibility by three authors (Karn Wijarnpreecha, Charat Thongprayoon and Patompong Ungprasert). Mutual agreement was used to solve controversy. For nonrandomized studies, Newcastle-Ottawa scale (13) was used to further appraise the publications in three areas including study selection, study comparison, and determination of the exposure for case-control study and outcome of interest for cohort study. For cross-sectional study, we classified each study by using adapted form of the Newcastle-Ottawa scale (14). The quality appraisal process was conducted by Karn Wijarnpreecha, Charat Thongprayoon and Patompong Ungprasert.
Data extraction
We obtained the following data from each article by using a standardized data collection form: last name of the first author’s, name of the study, year of publication, place where the study was conducted, number of subjects, demographics of subjects, diagnostic method of HBV infection, definition of CAD, diagnostic method of CAD, adjusted effect estimates with 95% CI and covariates that were adjusted in the multivariate analysis. To avoid errors, studies were assessed by the three authors independently. Data collection from for each study was cross-checked and was reported back to the original studies for data inconsistency.
Statistical analysis
For data analysis, we used Review Manager 5.3 software from the Cochrane Collaboration (London, UK). Pooled estimates and their standard errors from each study were analyzed by using generic inverse variance method as described by DerSimonian and Laird, which weighted each study according to its standard errors (15). For uncommon of outcome of interest, we used RR of cohort study as an estimate for OR to combine with OR from cross-sectional and case-control study. Since this meta-analysis combined data from three different study designs, we expected that between-study heterogeneity could be high and decided to use random-effect model, rather than fixed-effect model. Between-study heterogeneity was assessed by Cochran’s Q test which is complimented by I2 statistic. A value of I2 of 0–25% represents insignificant heterogeneity, 26–50% represents low heterogeneity, 51–75% represents moderate heterogeneity, and more than 75% represents high heterogeneity (16).
Results
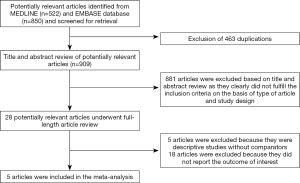
Of the 1,372 potential studies identified using our search strategy, 522 studies were from Medline and 850 studies were from EMBASE. We reviewed titles and abstracts of 909 studies after excluded 463 studies because of their repetition. A total of 881 studies were excluded at this stage since they were case reports, letters to editor, review articles, in vitro studies, animal studies or interventional studies. Twenty-eight studies underwent full-text article assessed for eligibility. Eighteen of them were excluded for absence of interest outcome while five studies were excluded since they were observational studies without comparison available. Therefore, a total of five studies, including three cross-sectional studies, one case-control study, and one cohort study, met the eligibility criteria and were subjected to analysis (8-12). Detailed literature retrieval, review and selection process are shown in Figure 1. Study characteristics and quality assessment are listed in Table 1. Preferred reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) is provided as Table S2 (17). The inter-rater agreement for the quality assessment using the Newcastle-Ottawa scale was high with the kappa statistics of 0.88.
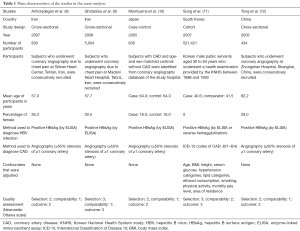
Full table

Full table
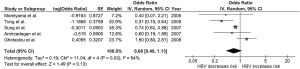
We found no significant association between HBV infection and risk of CAD with the pooled OR of 0.68 (95% CI, 0.40–1.13). There was moderate statistical heterogeneity between studies with an I2 of 64%. Figure 2 illustrated forest plot of this meta-analysis.
Evaluation for publication bias
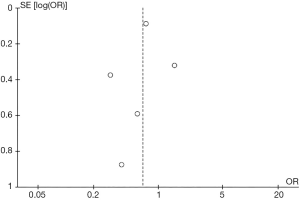
Funnel plot to evaluate publication bias is shown in Figure 3. The graph is fairly symmetric and provides no suggestion of publication bias.
Discussion
The association between chronic inflammation and accelerated atherosclerosis has long been recognized. In fact, studies have demonstrated an excess risk of CAD among HCV-infected patients compared with subjects without HCV infection (3,18). However, in this meta-analysis, we did not find a significant association between risk of CAD and HBV infection patients.
The reason behind the lack of association is unclear. It is possible that the inflammatory burden of chronic HBV infection is relatively low. In fact, a study has demonstrated that mean C-reactive protein levels among HBV-infected patients was not higher than HBV-seronegative individuals (8,9,12).
In contrast to studies on HCV infection that found an increased frequency of metabolic disturbance (19,20), studies of HBV-infected patients did not observed an increased prevalence of traditional risk factors of CAD including diabetes, hypertension, and hyperlipidemia (9). The absence of metabolic complication could be another factor for the lack of increased CAD risk among these patients.
Although most of the included studies were of high quality as reflected by the high quality assessment scores, we acknowledged that this meta-analysis had some limitations. Therefore, the results should be interpreted with caution.
First, the primary studies included in this meta-analysis were conducted primarily in Asia. Therefore, the results might not be generalizable to other populations with different baseline cardiovascular risk. Second, the heterogeneity was not low in this study. Third, most of the included studies did not adjust their effect estimates for several known risk factors for CAD such as diabetes, hyperlipidemia, and hypertension. Moreover, most of the included studies were cross-sectional in nature. Therefore, temporal relationship between HBV and CAD could not be established.
In summary, this meta-analysis did not demonstrate a significantly increased risk of CAD among HBV-infected patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation 2010;121:948-54. [Crossref] [PubMed]
- Mendis S, Abegunde D, Yusuf S, et al. WHO study on Prevention of REcurrences of Myocardial Infarction and StrokE (WHO-PREMISE). Bull World Health Organ 2005;83:820-9. [PubMed]
- Petta S, Maida M, Macaluso FS, et al. Hepatitis C Virus Infection Is Associated With Increased Cardiovascular Mortality: A Meta-Analysis of Observational Studies. Gastroenterology 2016;150:145-155.e4; quiz e15-6.
- Ungprasert P, Srivali N, Kittanamongkolchai W, et al. Risk of coronary artery disease in patients with ankylosing spondylitis: a systematic review and meta-analysis. Ann Transl Med 2015;3:51. [PubMed]
- Ungprasert P, Suksaranjit P, Spanuchart I, et al. Risk of coronary artery disease in patients with idiopathic inflammatory myopathies: a systematic review and meta-analysis of observational studies. Semin Arthritis Rheum 2014;44:63-7. [Crossref] [PubMed]
- Ungprasert P, Wijarnpreecha K, Ahuja W, et al. Coronary artery disease in primary biliary cirrhosis: A systematic review and meta-analysis of observational studies. Hepatol Res 2015;45:1055-61. [Crossref] [PubMed]
- Ott JJ, Stevens GA, Groeger J, et al. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine 2012;30:2212-9. [Crossref] [PubMed]
- Amirzadegan A, Davoodi G, Boroumand MA, et al. Association between hepatitis B surface antibody seropositivity and coronary artery disease. Indian J Med Sci 2007;61:648-55. [Crossref] [PubMed]
- Ghotaslou R, Aslanabadi N, Ghojazadeh M. Hepatitis B virus infection and the risk of coronary atherosclerosis. Ann Acad Med Singapore 2008;37:913-5. [PubMed]
- Momiyama Y, Ohmori R, Kato R, et al. Lack of any association between persistent hepatitis B or C virus infection and coronary artery disease. Atherosclerosis 2005;181:211-3. [Crossref] [PubMed]
- Sung J, Song YM, Choi YH, et al. Hepatitis B virus seropositivity and the risk of stroke and myocardial infarction. Stroke 2007;38:1436-41. [Crossref] [PubMed]
- Tong DY, Wang XH, Xu CF, et al. Hepatitis B virus infection and coronary atherosclerosis: results from a population with relatively high prevalence of hepatitis B virus. World J Gastroenterol 2005;11:1292-6. [Crossref] [PubMed]
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5. [Crossref] [PubMed]
- Herzog R, Álvarez-Pasquin MJ, Díaz C, et al. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health 2013;13:154. [Crossref] [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Crossref] [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336-41. [Crossref] [PubMed]
- Guiltinan AM, Kaidarova Z, Custer B, et al. Increased all-cause, liver, and cardiac mortality among hepatitis C virus-seropositive blood donors. Am J Epidemiol 2008;167:743-50. [Crossref] [PubMed]
- Petta S, Macaluso FS, Craxì A. Cardiovascular diseases and HCV infection: a simple association or more? Gut 2014;63:369-75. [Crossref] [PubMed]
- Younossi Z, Park H, Henry L, et al. Extrahepatic Manifestations of Hepatitis C: A Meta-analysis of Prevalence, Quality of Life, and Economic Burden. Gastroenterology 2016;150:1599-608. [Crossref] [PubMed]