Oscillating blood pressure therapeutic target in type 2 diabetes patients with hypertension
Introduction
Hypertension is the leading cause of cardiovascular disease (CVD) and deaths worldwide. Globally, hypertension affects more than 1 billion adults and cause at least 9 million deaths annually (1,2). Hypertension is very frequently associated with diabetes, with up to 70% of individuals with diabetes who are hypertensive (3). Coexistence of diabetes and hypertension is associated with increased cardiovascular morbidity and mortality (4). Thus, achieving tight blood pressure (BP) control in type 2 diabetes patients is paramount. In this context, guidelines and recommendations have been developed and updated to improve the clinical care and management of hypertension in type 2 diabetes patients. The most recent, the eight report from the Joint National Committee (JNC 8) guidelines have revisited and raised the threshold for initiating pharmacological treatment and goal in adult diabetes patients from 130/80 to 140/90 mmHg based on recent finding suggesting that an excessive reduction of BP can lead to an increase of cardiovascular events (5-7). This hypothesis called the “J shaped phenomenon” of BP control has generated many controversies (8). Although there are evidence suggesting that strong reduction of BP does not reduce the rate of a composite outcome of fatal and nonfatal major cardiovascular events in type 2 diabetes patients, it is important to consider that most of these evidence were drawn from studies presenting some confounding factors such as the presence of previous CVD and events and the increase in cardiovascular outcomes found with excessive lowering of BP appeared at a level of BP <110 mmHg, a quite outlier values used for the development of recommendations and very rarely seen in patients with hypertension taking conventional treatment (9). On the other hand, despite the fact that some randomized controlled trials suggest that excessive reduction of BP is associated with an increase in cardiovascular mortality (10,11), there is still little evidence that this mortality excess is due to BP lowering. The recent findings of the study by Adamsson Eryd et al. support this idea and relaunch the discussion on the J-shaped phenomenon of BP in type 2 diabetes patients (12).
Variety of BP target for hypertension treatment in diabetes patients
The JNC 8 report on management of high BP recommends in the population aged 18 years or older with diabetes to initiate antihypertensive pharmacologic treatment to lower BP at systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg (7). This report has been subject to many controversies since most of other scientific committees still recommend a lower threshold of BP in diabetes patients. The 2013 guidelines of ESC/ESH recommend to initiate pharmacological treatment for hypertension when BP >130/85 mmHg based on the need for early and aggressive intervention in order to reduce CVD risk in diabetes patients (6). On the other hand, the American Diabetes Association (ADA) in its most recent report on diabetes care standards recommends that patients with diabetes and hypertension should be treated to a SBP goal of 140/90 mmHg but recognize that lower BP targets, such as 130/80 mmHg, may be appropriate for certain individuals with diabetes (13). These differences found in guidelines underscore the very dynamic appearance of recommendations for public health issues such as hypertension and diabetes which are regularly modified.
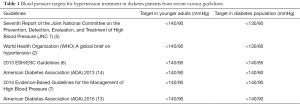
Evolution and key modifications in international guidelines of hypertension
The last decade has been the witness of many changes and modifications in international guidelines for the management of hypertensive diabetes patients with the aim of reducing their cardiovascular risk and mortality (Table 1). Despite the fact that all recommendations agree on the necessity of a tight BP control in diabetes patients in order to reduce macrovascular complications such as stroke, coronary artery diseases or heart failure, there are several differences in the threshold value for initiating pharmacological treatment and target BP value when treating. In 2004, the JNC 7 set the threshold defining hypertension in patients at high cardiovascular risk or presenting a major cardiovascular risk factor such as diabetes or chronic kidney disease at ≥130/80 mmHg (15). Most of the following international recommendations supported the fact that the definition of hypertension in diabetes patients should be different than that of general population to allow precocious and more efficient management of these conditions. Thus, the World Health Organization (WHO) guidelines agreed with this definition and recommend the same treatment goal for diabetes patients (16). In the same manner, the guidelines published by the ADA in 2013, changed and raised the BP targets in diabetes patients but maintained the need for lower DBP target in this population, setting the threshold for pharmacological treatment at 140/85 mmHg (14). But, some recent findings have led to the emerging theory of the J-curve phenomenon with reduction of BP, changing the so far conception that “lower is better” for BP (17,18). This hypothesis suggests a paradoxical increase in morbidity and mortality associated with an excessive reduction in BP (19). This fundamentally affects the management of BP with an increasing caution in the reduction of BP in diabetes patients. In this context, the JNC 8 report revisited the threshold value for defining and initiating hypertensive treatment in diabetes patients, increasing the set value to 140/90 mmHg. These modifications were assumed by the ADA with little difference recognizing the fact that threshold must be set at 130/80 mmHg for some diabetes individuals (13). The majority of these modifications especially those supporting the need to raise BP threshold for treatment in diabetes patients are supported by the principle of “primum non nocere” based on the possible existence of a J-shaped curve.
Full table
J-shaped Curve: starting point of controversy
Despite the fact that any increase in BP is strongly and directly related to vascular mortality in adult patients starting from 115/75 mmHg (20), and evidence that lowering BP was proven effective in preventing cardiovascular complications, many observational studies have reported an increase in cardiovascular death and events when very low BP values were reached in both treated and untreated hypertensive patients (21-23). These findings led to the hypothesis of the J-shaped curve of BP (22). This theory states that the relationship between BP and cardiovascular events is not linear but rather a J-shaped curve (19). This is could be either a physiologic or pathologic state or even a consequence of antihypertensive drug treatment. Physiological data supporting this hypothesis suggested that there must be a turning point of BP below which the risk of cardiovascular events increases, because BP is essential for the blood perfusion of all organs, such as the brain, heart, and kidneys. Post hoc analysis of observational studies emphasized that in individuals with a high or very high cardiovascular risk, excessive reduction of BP may lead to a nullification of the protective effect of BP lowering on cardiovascular mortality (8). The emergence of this hypothesis, the discussion and the questions it has raised are far from finished and there is need to clarify the pathophysiology of this phenomenon. While the majority of studies conducted in recent years confirm an increase in the number of cardiovascular events and increased mortality in patients with very low BP, the assumption that the J-curve is due to anti-hypertensive treatment and the veracity of this assumption in diabetes patients should still be subject to some reservations. There is little evidence drawn from well-randomized controlled trials of the existence of the J-curve after adjustment of all confounding factors at a level at BP is usually reached by classical anti-hypertensive therapy. The lack of randomization which failed to equally distribute adverse risk outcomes between groups and the low number of patients in the groups with very low BP significantly limit the reliability conclusions drawn from these studies and above all, their expansion to the rest of population via inferences (24). Furthermore, this phenomenon has been observed in placebo-treated groups supporting the idea that a J-curve if it does exist, is probably not the consequence of antihypertensive treatment (25). The increase in non-cardiovascular events unconnected with the decrease in BP also questions the causal effect of antihypertensive treatment in the appearance of a J-curve (26). On another side, major trials conducted in diabetes patients such as UKPDS and ACCORD studies did not provide any evidence or arguments in favor of the existence of a J-shaped curve when lower BP are achieved in adult diabetes patients (4,9).
Rationale for proofreading of previous evidence and guidelines for management of high BP in diabetes patients
A recent article published in British Medical Journal relaunches the debate on the J-shaped curve of hypertension especially in diabetes patients with no previous CVD (12). The authors compared the risk of cardiovascular events between patients from a large Swedish adult cohort (population size of 187,106; aged less than 75 years) assigned to six groups of systolic blood pressure: 110–119, 120–129, 130–139, 140–149, 150–159, and ≥160 mmHg. They reported a significant and continuous reduction of cardiovascular mortality and events with the reduction on BP without any evidence of J-shaped curve. They found that adults diabetes patients with no previous CVD and lower SBP between 110–119 mmHg had lower mortality rates and cardiovascular events than those with a SBP between 130–139 mmHg. Thus, in diabetes patients with no previous CVD, there is significant benefit in terms of cardiovascular mortality of lowering BP at a set less than 120 mmHg in contrary with the hypothesis of the J-shaped curve. Therefore, it stresses the need to revisit the fifth recommendation of the 2014 guidelines of the JNC 8 on hypertension treatment in diabetes patients. Indeed, this new evidence should be sufficient to reopen the debate on the J-shaped curve of hypertension especially in diabetes patients with no previous CVD.
Necessity to revisit the recent guidelines for hypertension in diabetes patients
First of all, we must take in consideration that most of the studies suggesting a J-curve shaped of hypertension were conducted in populations already presenting target organ damage such as stroke and/or coronary heart disease, therefore at greater risk of organ hypo-perfusion especially at low DBP (11,17,21,23,27,28). To date, to the best of our knowledge, there is no evidence that the increase in cardiovascular mortality found in these studies were all caused by anti-hypertensive therapy and not due to other confounding factors such as previous stroke, ischaemic heart disease or heart failure. This is supported by the study of Adamsson et al. which suggests that after adjustment for confounding factors such as previous CVD and age, the reduction of BP under 120 mmHg has no adverse outcomes (12). Moreover, the increase in cardiovascular events found in previous studies appears at a level of DBP lower than 70–80 mmHg or SBP lower than 100–110 mmHg which is 10–30 mmHg far from current guidelines targeting a BP of <140/90 mmHg (21,28). Yet, observational data suggested that, an increase of 20 mmHg in SBP or 10 mmHg in DBP is associated with a doubling of the risk of CVD death, regardless of age (29). Therefore, considering such a difference in cardiovascular risk in non-diabetes patients, associated to the fact that diabetes patients present higher cardiovascular risk than non-diabetic ones, there is a need to questioned the recent recommendations of the JNC8 which raised set value for initiating treatment from 130/80 to 140/90 mmHg in diabetes patients. On the other side, few studies supporting the J-shaped curve of BP were designed in young adults’ diabetes patients without other CVD. The ACCORD study, one of the major studies conducted in diabetes patients did not found any evidence of J-shaped curve of BP in diabetes patients at high risk for cardiovascular events while targeting a SBP of less than 120 mmHg, as compared with less than 140 mmHg. In addition, interpretation should be done with caution since, this branch of the study didn’t evaluate any benefit of excessive reduction of BP <120 mmHg on microvascular complications in regard to others organs such as kidneys and eyes (30). So, taking into consideration that high BP is also a risk factor for renal and ocular complications, if lowering BP in type 2 diabetes patients under 120 mmHg really has no benefit and no adverse outcomes on macrovascular complications, but could present an advantage regarding microvascular complications, it would be a sufficient argument for further reduction of BP in this population.
Another important point on which most studies results agree is the fact that sustained reduction and maintenance of BP of 10/5 mmHg around optimal BP is associated with the lower rate of cardiovascular events and mortality and not yet a J-shaped curve of cardiovascular events and mortality (4,20,21,23,28,29,31,32). So, even when the J-shaped curve would be proven in high risk populations without previous CVD, it will still not be an argument for targeting a BP with difference of more than 10/5 mmHg far from the optimal BP in these groups.
Finally, the controversial recommendation rising BP target from 130/80 to 140/90 mmHg was based on expert opinion and not on strong evidence as it must be the case (7). This stresses the need for more evidence to build such recommendations for a highly sensitive topic such as diabetes and hypertension association regarding their prevalence and their burden. The recently published paper by Adamsson Eryd et al. (12) provided an initial response and brings out the basis for further and similar research in this field to identify the real cause of J-shaped curve found in previous studies and to draw reliable conclusions based on strong evidence to support recommendations and guidelines for the management of high BP in adult diabetes population.
Conclusions
In the light of new evidence, there is a need to reopen the discussion about the J-shaped relationship between BP reduction and mortality. Indeed, the paradoxical increase in mortality associated with low BP could be due to concomitant disease rather than antihypertensive treatment. Lower BP than currently recommended might be associated with significantly lower risk of cardiovascular events in diabetes patients.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60. [Crossref] [PubMed]
- World Health Organization. A global brief on hypertension. Available online: http://ish-world.com/downloads/pdf/global_brief_hypertension.pdf
- Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension 2001;37:1053-9. [Crossref] [PubMed]
- Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412-9. [Crossref] [PubMed]
- National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure [Internet]. Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2004 [cited 2016 Sep 21]. Available online: http://www.ncbi.nlm.nih.gov/books/NBK9630/
- Task Force for the management of arterial hypertension of the European Society of Hypertension; Task Force for the management of arterial hypertension of the European Society of Cardiology. 2013 ESH/ESC Guidelines for the Management of Arterial Hypertension. Blood Press 2013;22:193-278. [Crossref] [PubMed]
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20. [Crossref] [PubMed]
- Kang YY, Wang JG. The J-Curve Phenomenon in Hypertension. Pulse (Basel) 2016;4:49-60. [Crossref] [PubMed]
- Mancia G. Effects of intensive blood pressure control in the management of patients with type 2 diabetes mellitus in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Circulation 2010;122:847-9. [Crossref] [PubMed]
- Falcone C, Matrone B, Bozzini S, et al. Time-domain heart rate variability in coronary artery disease patients affected by thyroid dysfunction. Int Heart J 2014;55:33-8. [Crossref] [PubMed]
- Messerli FH, Mancia G, Conti CR, et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med 2006;144:884-93. [Crossref] [PubMed]
- Adamsson Eryd S, Gudbjörnsdottir S, Manhem K, et al. Blood pressure and complications in individuals with type 2 diabetes and no previous cardiovascular disease: national population based cohort study. BMJ 2016;354:i4070. [Crossref] [PubMed]
- Standards of Medical Care in Diabetes-2016 Summary of Revisions. Diabetes Care 2016;39 Suppl 1:S4-5. [Crossref] [PubMed]
- American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care. 2013;36 Suppl 1:S11-66. [Crossref] [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560-72. [Crossref] [PubMed]
- Gabb GM, Mangoni AA, Anderson CS, et al. Guideline for the diagnosis and management of hypertension in adults - 2016. Med J Aust 2016;205:85-9. [Crossref] [PubMed]
- Dorresteijn JA, van der Graaf Y, Spiering W, et al. Relation between blood pressure and vascular events and mortality in patients with manifest vascular disease: J-curve revisited. Hypertension 2012;59:14-21. [Crossref] [PubMed]
- Cruickshank JM. Coronary flow reserve and the J curve relation between diastolic blood pressure and myocardial infarction. BMJ 1988;297:1227-30. [Crossref] [PubMed]
- Mancia G, Grassi G. Aggressive blood pressure lowering is dangerous: the J-curve: pro side of the arguement. Hypertension 2014;63:29-36. [Crossref] [PubMed]
- Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903-13. [Crossref] [PubMed]
- D'Agostino RB, Belanger AJ, Kannel WB, et al. Relation of low diastolic blood pressure to coronary heart disease death in presence of myocardial infarction: the Framingham Study. BMJ 1991;303:385-9. [Crossref] [PubMed]
- Boutitie F, Gueyffier F, Pocock S, et al. J-shaped relationship between blood pressure and mortality in hypertensive patients: new insights from a meta-analysis of individual-patient data. Ann Intern Med 2002;136:438-48. [Crossref] [PubMed]
- Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA 2010;304:61-8. [Crossref] [PubMed]
- Verdecchia P, Angeli F, Mazzotta G, et al. Aggressive blood pressure lowering is dangerous: the J-curve: con side of the arguement. Hypertension 2014;63:37-40. [Crossref] [PubMed]
- Fagard RH, Staessen JA, Thijs L, et al. On-treatment diastolic blood pressure and prognosis in systolic hypertension. Arch Intern Med 2007;167:1884-91. [Crossref] [PubMed]
- Boutitie F, Gueyffier F, Pocock S, et al. J-shaped relationship between blood pressure and mortality in hypertensive patients: new insights from a meta-analysis of individual-patient data. Ann Intern Med 2002;136:438-48. [Crossref] [PubMed]
- Sleight P, Redon J, Verdecchia P, et al. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens 2009;27:1360-9. [Crossref] [PubMed]
- Bangalore S, Qin J, Sloan S, et al. What is the optimal blood pressure in patients after acute coronary syndromes?: Relationship of blood pressure and cardiovascular events in the PRavastatin OR atorVastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction (PROVE IT-TIMI) 22 trial. Circulation 2010;122:2142-51. [Crossref] [PubMed]
- Kovell LC, Ahmed HM, Misra S, et al. US Hypertension Management Guidelines: A Review of the Recent Past and Recommendations for the Future. J Am Heart Assoc. 2015.4. [PubMed]
- ACCORD Study Group, Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575-85. [Crossref] [PubMed]
- Stewart IM. Relation of reduction in pressure to first myocardial infarction in patients receiving treatment for severe hypertension. Lancet 1979;1:861-5. [Crossref] [PubMed]
- Bangalore S, Messerli FH, Wun CC, et al. J-curve revisited: An analysis of blood pressure and cardiovascular events in the Treating to New Targets (TNT) Trial. Eur Heart J 2010;31:2897-908. [Crossref] [PubMed]


