Non-intubated simultaneous en bloc resection of pulmonary nodule and rib chondrosarcoma
Introduction
Radical en bloc resection with disease-free margin of the whole tumor is the mainstay of therapy for chest wall chondrosarcoma to minimize recurrence rate, which tends to be resistant to conventional chemo-radiotherapy (1). Non-intubated chest surgery using regional anesthesia demonstrated less anesthesia-related pulmonary complications and notably faster recovery (2,3). Here a case was presented, who underwent simultaneous uniport thoracoscopic pulmonary wedge resection and en bloc resection of rib chondrosarcoma under local anesthesia without double-lumen endotracheal intubation, to tentatively evaluate its feasibility and safety.
Case presentation
A 61-year-old woman was admitted for a palpable giant mass on right side of the chest wall for more than 20 years, with mild swelling pain for 5 years after a chest trauma. The lesion was diagnosed as chondroma 20 years ago by needle biopsy, which was growing rapidly from approximately 5 cm × 5 cm to 12 cm × 9 cm in recent 5 years. The chest computed tomography (CT) scan revealed an irregular mass with mixed density which had penetrated into thorax through the 7th rib (Figure 1), with concurrent solitary pulmonary nodule in left upper lobe about 0.9 cm × 0.8 cm (Figure 2), besides, cranial magnetic resonance, abdominal CT and bone ECT excluded other metastatic lesions. Because rib chondrosarcoma and pulmonary metastasis was suspected, needle biopsy was not performed to avoid possible tumor dissemination. This patient could tolerate tracheal intubation and general anesthesia with normal cardiopulmonary function, and the decision of non-intubated surgery was made on the basis of several reports (2,3), which demonstrated the advantages of non-intubated procedure compared with intubated surgery. And it was approved by Ethics Committee of Xuzhou Central Hospital.

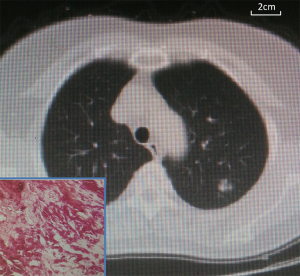
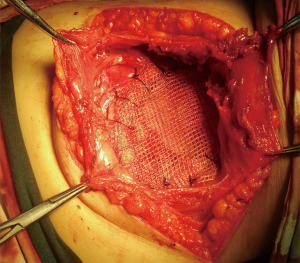
Firstly, instead of general anesthesia, uniport thoracoscopic pulmonary wedge resection assisted with CO2 artificial pneumothorax without endotracheal intubation was performed, utilizing local intercostal nerve block combined with intravenous propofol sedation under spontaneous breathing, and the intrathoracic pressure was maintained at 12 mmHg. Beside, 40% oxygen was delivered at 3.5 mL/min using a laryngeal mask, and the anesthesia depth was measured by electroencephalographic (EEG) bispectral index during the surgery, and devices for tracheal intubation and mechanical ventilation were prepared in case emergency for surgical safety as reported (2). Subsequently, the giant rib malignancy was resected en bloc carefully to avoid rupture as there was no regular capsule. CT reconstruction and simulated surgery was utilized for disease-free surgical margin (R0 resection), and partial anterior part of 7th rib was resected with the whole mass, with approximately 4 cm safety margin from the tumor, then the anterior chest wall was reconstructed with double composite mesh, which was fixed to the surrounding muscles and the remaining rib (Figure 3). The total operation lasted for 4.5 hours with intraoperative blood loss about 200 mL. Then the patient-controlled intravenous analgesia was administrated for 2 days. In addition, the hemodynamic index including PaO2, PaCO2 and central venous pressure were stable throughout the surgery. Besides, the recovery was mainly uneventful, and the patient returned to normal activities 6 hours after surgery without hemoptysis, palpitation, dyspnea or vomiting, except for moderate chest pain, and she discharged 7 days after the surgery. Furthermore, pulmonary inflammatory pseudotumor was diagnosed by hematoxylin and eosin (H&E) staining, and histologically highly differentiated (grade I) rib chondrosarcoma was confirmed by immunohistochemistry, with negative surgical margin (R0 resection), which was repeatedly verified by different pathologists. Moreover, neither intensity-modulated radiotherapy nor chemotherapy was recommended by multidisciplinary therapeutic consultants, as it was insensitive to conventional chemo- and radiotherapy as reported (1). Then the patient was followed up remotely utilizing internet-based approaches with life-style intervention and psychological support for 2 months, who demonstrated satisfactory life quality evaluated by 36-Item Short Form Health Survey without local recurrence.
Discussion
Chondrosarcoma is the most common primary tumor of the chest wall, and risk factors for survival of patients include extracompartmental spread, local recurrence and high histological grade (poorly differentiated), while risk factors for local recurrence include inadequate surgical margins and tumor size >10 cm (4). In addition, it was reported that all the patients with grade I pelvic chondrosarcoma developed a local recurrence after intralesional resection, whereas no patient received local relapse with wide resection margins (5). As fine-needle aspiration cytology is not proper because of local dissemination risk, wide surgical excision with tumor-free margins (en bloc, R0) is the mainstay of therapy for rib chondrosarcoma (6). Furthermore, lung is the most common metastasis site of chondrosarcoma (7). Although PET/CT might be the most reasonable choice for preoperative staging of this patient, it was expensive. In presenting case, pulmonary nodule with suspicious of metastasis was resected simultaneously, which turned out to be inflammatory pseudotumor. It is noteworthy that free margin of the rib is hard to decide intraoperatively, thus, preoperative simulated resection using 3D-CT or rapid prototyping of chest wall as reported could be facilitated to minimize the tumor contamination with safe anatomical margin (8).
Non-intubated surgical procedure was aimed to minimize the adverse effects of endotracheal intubation and general anesthesia, such as intubation-related airway trauma, ventilation-induced lung injury, residual neuromuscular blockade, and postoperative nausea and vomiting (9), especially for patients with tracheal intubation and general anesthesia related risks. Preliminary reports had suggested optimal feasibility of non-intubated procedure for pulmonary wedge resection, lung volume reduction surgery for severe emphysema and anatomical lung resection for lung cancer (10), and non-intubated surgery under epidural anesthesia demonstrated significantly less antibiotic use and hospital stay with decreased inflammatory cytokines, compared with general anesthesia and double-lumen endotracheal intubation (3). Besides, non-intubated thoracoscopic lung biopsy and chest drainage by local anesthesia and sedation was well tolerated and safe for patients aged 80 years and older (11). Moreover, the anesthesia techniques for non-intubated procedures include local wound infiltration, thoracic wall blocks, selective intercostal nerve blockade, thoracic paravertebral blockade and thoracic epidural analgesia (12).
On the other hand, noninvasive ventilation for patients with respiratory failure from severe asthma exacerbation remains controversial (13), and a low expired tidal volume is almost impossible in patients receiving noninvasive ventilation for de novo acute hypoxemic respiratory failure (14). However, a multicenter, randomized, parallel-group clinical trial indicated that noninvasive ventilation using facial mask for patients with hypoxemic respiratory failure was associated with significantly more invasive ventilation-free days and fewer health care-associated infections, compared with standard oxygen therapy (15). Furthermore, it was reported that non-intubated procedure should be avoided for certain conditions including low cardiac output, heart failure, overweight or obesity, pulmonary insufficiency with or without poorly controlled asthma, severe pleural adhesions and hemodynamic instability, etc. (2).
In conclusion, the feasibility and safety of non-intubated simultaneous en bloc resection of pulmonary nodule and chest wall chondrosarcoma by local intercostal nerve block under spontaneous breathing was tentatively evaluated from this presenting case, and life-quality oriented remote interventions using internet indicated satisfactory response from the patient. Nevertheless, multicenter, large-scale studies concerning inclusion/exclusion criteria, reference standard for risk-benefit evaluation of non-intubated surgery are required.
Acknowledgements
Funding: This study was supported by Speciality Fund for Jiangsu Key Laboratory of Molecular and Translational Cancer Research (No. BM2013007).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Martini N, Huvos AG, Burt ME, et al. Predictors of survival in malignant tumors of the sternum. J Thorac Cardiovasc Surg 1996;111:96-105; discussion 105-6. [Crossref] [PubMed]
- Liu J, Li S, Shen J, et al. Non-intubated resection and reconstruction of trachea for the treatment of a mass in the upper trachea. J Thorac Dis 2016;8:594-9. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Fiorenza F, Abudu A, Grimer RJ, et al. Risk factors for survival and local control in chondrosarcoma of bone. J Bone Joint Surg Br 2002;84:93-9. [Crossref] [PubMed]
- Streitbürger A, Ahrens H, Balke M, et al. Grade I chondrosarcoma of bone: the Münster experience. J Cancer Res Clin Oncol 2009;135:543-50. [Crossref] [PubMed]
- Roos E, van Coevorden F, Verhoef C, et al. Prognosis of Primary and Recurrent Chondrosarcoma of the Rib. Ann Surg Oncol 2016;23:811-7. [Crossref] [PubMed]
- Al-Refaie RE, Amer S, Ismail MF, et al. Chondrosarcoma of the chest wall: single-center experience. Asian Cardiovasc Thorac Ann 2014;22:829-34. [Crossref] [PubMed]
- Kurenov SN, Ionita C, Sammons D, et al. Three-dimensional printing to facilitate anatomic study, device development, simulation, and planning in thoracic surgery. J Thorac Cardiovasc Surg 2015;149:973-9.e1. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Pompeo E. State of the art and perspectives in non-intubated thoracic surgery. Ann Transl Med 2014;2:106. [PubMed]
- Katlic MR, Facktor MA. Non-intubated video-assisted thoracic surgery in patients aged 80 years and older. Ann Transl Med 2015;3:101. [PubMed]
- Kiss G, Castillo M. Non-intubated anesthesia in thoracic surgery-technical issues. Ann Transl Med 2015;3:109. [PubMed]
- Bahloul M, Chtara K, Gargouri R, et al. Failure of noninvasive ventilation in adult patients with acute asthma exacerbation. J Thorac Dis 2016;8:744-7. [Crossref] [PubMed]
- Carteaux G, Millán-Guilarte T, De Prost N, et al. Failure of Noninvasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume. Crit Care Med 2016;44:282-90. [Crossref] [PubMed]
- Jaber S, Lescot T, Futier E, et al. Effect of Noninvasive Ventilation on Tracheal Reintubation Among Patients With Hypoxemic Respiratory Failure Following Abdominal Surgery: A Randomized Clinical Trial. JAMA 2016;315:1345-53. [Crossref] [PubMed]


