Current understanding in source control management in septic shock patients: a review
Introduction
Source control is an old term that makes reference to one of the oldest way for controlling an ongoing infection, records from ancient Egypt already mentioned the drainage of thoracic abscess as a source control measure (1). It involves all physical actions taken in the process of care to control a focus of infection and subsequently reduce the favorable conditions that promote microorganism growth or that keep impaired host defenses (2). The importance of source control has been retaken with the surviving sepsis campaign (3), however last recommendations (4) only make four statements on this matter, with low evidence grade endorsing a gap of 12 hours for its achievement when feasible. Most recent studies make emphasis in antibiotics (time, dose) organ support therapies, reanimation (crystalloids versus colloids, vasopressors) and more recently adjuvant strategies for septic patients, however evidence in the oldest manner to control an infection is scarce. Source control is a cornerstone in the treatment of infectious diseases and it becomes an urgent matter in septic shock patients. Here the authors present a review on the rationale of source control, recent recommendations in this matter and future directions for trials or research.
Rationale for source control
The process of infection is a complex state that involves both microorganism and host mechanisms to prevail. A local initial inflammatory responds attracts neutrophils, macrophages, and other phagocytes promotes the release of cytokines such as IL-8, IL-1 and the activation of the coagulation cascade. In some cases this is accompanied by liquefaction necrosis and the release of pus with replicating microorganism in this site. Defensive host responses include the formation of fibrin deposits to shield healthy tissues from the dissemination, establishing an abscess (5). This abscess will protect both host and bug, where no drug will penetrate well enough to control the infection. Some other forms of persistent foci of infection have become evident with advances in modern care, aging, comorbidities, invasive procedures, chronic care facilities and in day hospitals have made that some specific population could present differently from abscess alone or with multidrug resistant microorganisms.
This local, initial process is common for almost all complicated soft tissue infections and some of intra-abdominal septic shock patients, and is what gives the basis for source control in those, whereas (I) drainage of infected fluid collections; (II) debridement of infected solid tissue and the removal of devices or foreign bodies; and (III) definitive measures to correct anatomic derangements resulting in ongoing microbial contamination and to restore optimal function conform actions included under this definition and will contribute on outcome (6,7).
Soft tissue and skin infections
This kind of infections represent the third most frequent cause of severe sepsis and septic shock following pneumonia and intra-abdominal infections (IAIs) in some series (8,9), but one of those that source control measures can be more evident. The spectre of diseases that are included in this group can presents differently and so categorized, according to causative microorganism, or extension or clinical symptoms. A clinical categorization depending on presence of septic shock and the urgency of requirement for surgical procedures in order to achieve source control has been described (10) with worst outcomes in those with inadequate therapy and sepsis. Source control in these infections comprises since topical actions, incision and drainage, debridement, up to amputation. Patients at intensive care unit (ICU) with severe soft tissue and skin infection are mostly represented by those with necrotizing fasciitis (NF), and many times with organ failure associated. Recent recommendations on the approach regarding NF (11) states that in uncertain cases time should not be wasted in extensive clinical diagnosis, or scoring severity of the patient or hesitating on extension of the first incision. A deep incision up to the fascia should be performed and if NF is diagnosed, radical debridement should be implemented. Recent guidelines (12,13) on the management of soft tissue and skin infections make recommendations on prompt and extensive surgery, and a second debridement when necessary to discard ongoing local extension, among the use of broad spectrum antibiotics. Seems prudent that, whenever possible, source control should be attempted as soon as foci is detected. A delayed first surgical intervention (more than 12 hours) is associated with higher mortality (14), however in a recent report (15) an early intervention (less than 6 hours from diagnosis) was associated with shorter ICU and hospital length of stay but no statistical differences in mortality were founded between early and late surgery. Antibiotics should be given as any septic shock patient in the first 6 hours, and administration of clindamycin is highly recommended in order to inhibit exotoxin production of Gram-positive bacteria. Duration of antibiotic treatment can be between 7–14 days according to guidelines (12,13).
IAIs
IAIs are the second cause of admission to the ICU in large series (16,17). The number of cases of peritonitis that required admission to an ICU due to organ failure had remained stable during time both community-acquired and nosocomial-related, however this latter group seems to be increasing in recent reports (18). IAI commonly represents the other group of septic shock patients that have an identified foci of infection where source control actions become feasible besides skin and soft tissues infection (7,19-21). As any other supportive action in septic shock patient time is an urgent matter. Time between admission and source control in IAI has been assessed as a critical determinant of survival in patients with GI perforation with associated septic shock (22), and in some intra-abdominal candidiasis cases (23), however in these reports “early” goes from 2 hours up to 5 days.
The quality of source control is difficult to evaluate (24,25) IAIs without it, mortality probably could reach up to 100% (26). The appropriate interventions to determine the adequacy of source control are dictated by the clinical circumstances. High risk patients as such in septic shock with high doses of inotropes or requiring other supportive measures could benefit for new approaches. Nowadays minimal invasive procedures including percutaneous and endoscopic treatments have been described for non-severe cases. It may have a role in well localized abscesses or in surgical inaccessible abdomen. Recent recommendations on source control and peritonitis use the term “damage control” surgery for this kind of critically ill patients with inaccessible abdomen (26). Surgery gives opportunity to take first local microbiological samples however some interventions may cause further complications and risk factors associated with the procedures. Current guidelines on the management of IAIs (21,27) discourage systematic reoperations as routine practice. In the other hand assuming risks for patients in septic shock to be carried to the operating room (OR) and the best moment for to take this measures is difficult to assess and evaluate, transfer, surgery, anaesthesia are some of the key players to address. Table 1 resumes source control actions in skin and soft tissue and IAIs.
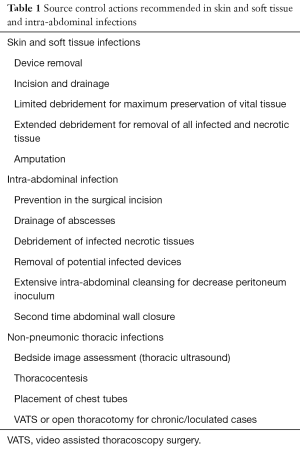
Full table
Non-pneumonic thoracic infection
Pleural infection is a non-rare complication for pneumonia, almost 20% of these empyema episodes will require surgical intervention as source control measure (28). Every patients presenting with a pleural effusion in association with sepsis or pneumonic illness require a prompt diagnostic pleural fluid sampling. In recent years, to employ thoracic ultrasound at the bedside to determine the presence of effusions especially in septic shock patients at the ICU has increased. It is a safe, fast and effective tool to determine volume and accessibility in order to drain abscesses or pleural infected effusions. Recent recommendations on this matter (29,30) suggested as first approach the use of thoracic ecography, following diagnostic sampling thoracocentesis, and if necessary the placement of a chest tube. The role of video assisted thoracoscopy and open thoracotomy can be reserved for those chronic or loculated cases.
Mediastinitis is a more difficult to approach infection due to anatomical difficulties, there are discrepancies whether time and surgical approach will lead to better outcomes. A recent large review of descending necrotizing mediastinitis (31) suggested that a prompt and aggressive surgical treatment was related with survival and in extended cases the transthoracic approach was recommended.
Urinary tract infections
This group of infections account for the third or fourth group of infections admitted to the ICU depending on different reports. It seems of common sense that in those where an abscess is identified or where an obstruction in the usual urinary flow (obstructive pyelonephritis) is the responsible for the infection; the prompt action taken to solve this (drainage or lithotomy and placement of catheters) are recommended as source control measures as mentioned above. A concerning issue are the catheter associated urinary tract infections a common problem in both ICU and non-ICU patients (32) more so because of it probability of preventing it. However a recent multicenter analysis (33) based on an educational program addressing many of the factors involved in this type of infection showed that these programs are efficient only on non-ICU patients when compared to ICU patients in decreasing both use and related infection.
Some other sites of infection such as pneumonia, or bacteremia have a more difficult to achieve source control goals, so probably in this patients, the importance of the correct and prompt initiation of antibiotics along with support measures have a larger effect in their outcome, however further trials are required in this matter.
Conclusions
Source control remains as a cornerstone in the treatment of septic shock patients. IAIs along with soft tissues infections are the sites where a rapid source control seems more feasible. Recommendations and educational efforts should advise a more prompt achievement of source control.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jungraithmayr W, Weder W. Chest surgical disorders in ancient Egypt: evidence of advanced knowledge. Ann Surg 2012;255:605-8. [Crossref] [PubMed]
- Marshall JC, Al Naqbi A. Principles of source control in the management of sepsis. Crit Care Nurs Clin North Am 2011;23:99-114. [Crossref] [PubMed]
- Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Intensive Care Med 2004;30:536-55. [Crossref] [PubMed]
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013;41:580-637. [Crossref] [PubMed]
- Misiakos EP, Bagias G, Patapis P, et al. Current concepts in the management of necrotizing fasciitis. Front Surg 2014;1:36. [Crossref] [PubMed]
- Jimenez MF, Marshall JC. International Sepsis Forum. Source control in the management of sepsis. Intensive Care Med 2001;27 Suppl 1:S49-62. [Crossref] [PubMed]
- Marshall JC, Maier RV, Jimenez M, et al. Source control in the management of severe sepsis and septic shock: an evidence-based review. Crit Care Med 2004;32:S513-26. [Crossref] [PubMed]
- Shen HN, Lu CL. Skin and soft tissue infections in hospitalized and critically ill patients: a nationwide population-based study. BMC Infect Dis 2010;10:151. [Crossref] [PubMed]
- Engel C, Brunkhorst FM, Bone HG, et al. Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med 2007;33:606-18. [Crossref] [PubMed]
- Marwick C, Broomhall J, McCowan C, et al. Severity assessment of skin and soft tissue infections: cohort study of management and outcomes for hospitalized patients. J Antimicrob Chemother 2011;66:387-97. [Crossref] [PubMed]
- Eckmann C. The importance of source control in the management of severe skin and soft tissue infections. Curr Opin Infect Dis 2016;29:139-44. [Crossref] [PubMed]
- Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious diseases society of America. Clin Infect Dis 2014;59:147-59. [Crossref] [PubMed]
- Sartelli M, Malangoni MA, May AK, et al. World Society of Emergency Surgery (WSES) guidelines for management of skin and soft tissue infections. World J Emerg Surg 2014;9:57. [Crossref] [PubMed]
- Kobayashi L, Konstantinidis A, Shackelford S, et al. Necrotizing soft tissue infections: delayed surgical treatment is associated with increased number of surgical debridements and morbidity. J Trauma 2011;71:1400-5. [Crossref] [PubMed]
- Hadeed GJ, Smith J, O'Keeffe T, et al. Early surgical intervention and its impact on patients presenting with necrotizing soft tissue infections: A single academic center experience. J Emerg Trauma Shock 2016;9:22-7. [Crossref] [PubMed]
- Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009;302:2323-9. [Crossref] [PubMed]
- De Waele J, Lipman J, Sakr Y, et al. Abdominal infections in the intensive care unit: characteristics, treatment and determinants of outcome. BMC Infect Dis 2014;14:420. [Crossref] [PubMed]
- Inui T, Haridas M, Claridge JA, et al. Mortality for intra-abdominal infection is associated with intrinsic risk factors rather than the source of infection. Surgery 2009;146:654-61; discussion 661-2. [Crossref] [PubMed]
- Bader FG, Schröder M, Kujath P, et al. Diffuse postoperative peritonitis -- value of diagnostic parameters and impact of early indication for relaparotomy. Eur J Med Res 2009;14:491-6. [Crossref] [PubMed]
- Pieracci FM, Barie PS. Intra-abdominal infections. Curr Opin Crit Care 2007;13:440-9. [Crossref] [PubMed]
- Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis 2010;50:133-64. [Crossref] [PubMed]
- Azuhata T, Kinoshita K, Kawano D, et al. Time from admission to initiation of surgery for source control is a critical determinant of survival in patients with gastrointestinal perforation with associated septic shock. Crit Care 2014;18:R87. [Crossref] [PubMed]
- Vergidis P, Clancy CJ, Shields RK, et al. Intra-Abdominal Candidiasis: The Importance of Early Source Control and Antifungal Treatment. PLoS One 2016;11:e0153247. [Crossref] [PubMed]
- Tellor B, Skrupky LP, Symons W, et al. Inadequate Source Control and Inappropriate Antibiotics are Key Determinants of Mortality in Patients with Intra-Abdominal Sepsis and Associated Bacteremia. Surg Infect (Larchmt) 2015;16:785-93. [Crossref] [PubMed]
- Solomkin JS, Ristagno RL, Das AF, et al. Source control review in clinical trials of anti-infective agents in complicated intra-abdominal infections. Clin Infect Dis 2013;56:1765-73. [Crossref] [PubMed]
- Montravers P, Blot S, Dimopoulos G, et al. Therapeutic management of peritonitis: a comprehensive guide for intensivists. Intensive Care Med 2016;42:1234-47. [Crossref] [PubMed]
- Montravers P, Dupont H, Leone M, et al. Guidelines for management of intra-abdominal infections. Anaesth Crit Care Pain Med 2015;34:117-30. [Crossref] [PubMed]
- Finley C, Clifton J, Fitzgerald JM, et al. Empyema: an increasing concern in Canada. Can Respir J 2008;15:85-9. [Crossref] [PubMed]
- Davies HE, Davies RJ, Davies CW, et al. Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii41-53. [Crossref] [PubMed]
- Scarci M, Abah U, Solli P, et al. EACTS expert consensus statement for surgical management of pleural empyema. Eur J Cardiothorac Surg 2015;48:642-53. [Crossref] [PubMed]
- Bayarri Lara CI, Sevilla López S, Sánchez-Palencia Ramos A, et al. Surgical management of descending necrotizing mediastinitis. Cir Esp 2013;91:579-83. [Crossref] [PubMed]
- Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 2014;370:1198-208. [Crossref] [PubMed]
- Saint S, Greene MT, Krein SL, et al. A Program to Prevent Catheter-Associated Urinary Tract Infection in Acute Care. N Engl J Med 2016;374:2111-9. [Crossref] [PubMed]


