Outcomes of off-pump versus on-pump coronary artery bypass graft surgery in patients with severely dilated left ventricle
Introduction
Coronary artery disease (CAD) is the major cause of mortality in the world. Atherosclerotic disease of the epicardial coronary arteries is an excessive, inflammatory-fibroproliferative response (1), leading to narrowing of the lumen of these vessels and subsequent reduction of blood supply to the myocardium, resulting in myocardial ischemia, acute myocardial infarction (MI) and often death. Despite the huge advancement of percutaneous revascularization, bypass surgery is still a treatment of choice in most patients with coronary disease. To large extent, the surgery reduces the recurrence of myocardial ischemia and the demand of revascularization (2). For elderly patients and patients with diabetes mellitus, renal insufficiency, poor left ventricular ejection fraction (LVEF) (≤35%), peripheral vascular disease, left main CAD and chronic obstructive pulmonary disease (COPD), off-pump coronary artery bypass (OPCAB) grafting is associated with lower operative combination and mortality than on-pump coronary artery bypass (ONCAB) (3-6). For patients with giant left ventricle, few reports are available (7). The objective of this retrospective study was to examine the safety and applicability of OPCAB in patients with giant left ventricle and to discuss the clinical implications for surgical methods.
Methods
Study patients
A total of 50 patients with severely dilated left ventricle [left ventricular end diastolic diameter (LVEDD) ≥ VE mm] underwent isolated myocardial-revascularization from 2009 through 2015 were included. This study was approved by the Regional Ethics Committee of Shanghai Jiao Tong University and informed consents were obtained from all patients. Patients were received either ONCABG (n=24) or OPCAB (n=26). All the operations were performed by same surgical team. Routinely, we offered patients aspirin, β-block, low fraction heparin for poor cardiac function patient and positive inotropic agents were administrated before surgery.
Surgical procedures
Surgery was carried out via a median sternotomy either with cardiopulmonary bypass (CPB) or the off-pump technique. ONCAB was practiced with administration of cardio-pulmonary bypass technique and proximal anastomosis was finished with cross-clamping of the aorta. To achieve an active clotting time (ACT) in excess of 480 s with additional heparin as required, systemic heparinisation was given (3 mg/kg). After the aortic and atrial cannulation was accomplished, the locations of planned distal anastomoses were marked with a scalpel. To arrest the heart in diastole, antegrade cold blood (4 °C) cardioplegic solution was administered via aortic root and grafts. And the ice was positioned to the epicardium to protect the myocardium. Arteriotomy sites should be chosen proximal enough to offer the largest-sized coronary target but distal enough to avoid areas of obstruction or significant atherosclerotic disease. After the accomplishment of the last distal anastomosis, the patient was separated from CPB when the patient’s temperature was greater than 36.5 °C. Then, the protamine sulfate was administered to reverse the additional heparin. The sternum was closed after surgical field was carefully stanched.
For OPCAB procedure, systemic heparinisation was administered (0.8 mg/kg), and ACT greater than 280 s was maintained. In order to achieve a satisfied myocardial exposure, surgical sponges was damped behind the heart and deep pericardial tension suture was placed. After the pericardium was fixed, a stabilizer (octopus 4 tissue stabilizer, Medtronic, Minneapolis, USA) was applied for target vessel exposal. Shunt (ClearView Intracoronary Shunt, Medtronic, Minneapolis, USA) was inserted to maintain the distal perfusion during anastomosis and a mister blower (Guidant, Indianapolis, USA) with CO2 water was applied to provide a blood-less field. After the surgery was done, protamine was added to reverse the excessive of heparin and the sternum was closed by steel wire.
Follow-up
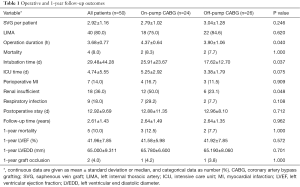
An up-to-date clinical follow-up was obtained by a telephonic interview with the patient or her/his family. The occurrence of at least one postoperative major adverse cardiac and cerebrovascular event (MACCE)—defined as any of the following complications from hospital discharge to follow-up: sudden death, recurrent angina, MI, congestive heart failure, percutaneous coronary intervention, repeat coronary artery bypass grafting (CABG) and cerebrovascular accident—was recorded. Follow-up data are shown in Table 1 and were collected till December 2015 (up to 6 years). Median follow-up time was 28 (range, 12–72) months. There were 20 cases (83.3%) in ONCAB group and 23 (88.5%) in the OPCAB group alive during follow-up. And 1-year coronary computed tomography angiography (CCTA) was carried out to evaluate the patency of the graft for each patients.
Full table
Statistical analysis
Statistical analyses were performed using SPSS v22 for Windows (SPSS Corp., Birmingham, AL, USA). Categorical data were presented as percentages and were analysed using the Chi square test or Fisher’s exact test. Continuous data are presented as means and standard deviations. Long-term survival was estimated by Kaplan-Meier curves and analysed with the long-rank test. A level of significance P<0.05 was considered significant. Propensity matching was attempted but the two groups could not be matched due to small numbers in both groups.
Results
Baseline characteristics and in-hospital outcomes
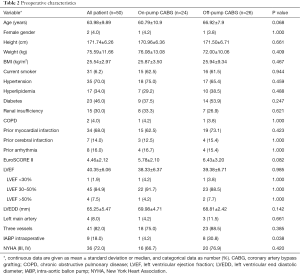
Demographics of two patient populations are shown in Table 2. In comparison to the ONCAB group, there were more intra-aortic ballon pump (IABP) insertion in patients undergoing Off-pump surgery (P<0.05). Sex, age, hypertension, hyperlipidemia, diabetes mellitus, renal dysfunction, COPD, previously myocardial infraction, arrhythmia, EuroSCORE II, LVEF, pre-procedural LVEDD were no significant difference between two groups (P>0.05). Mean ± SD LVEDD was 68.81±2.42 mm in the OPCAB group and 69.98±4.71 mm in the ONCAB group. Comparing to OPCAB, ONCAB required longer operation time, post-surgery intubation time and more renal dysfunction (P<0.05). There was no significant difference between perioperative period myocardial infraction, intensive care unit (ICU) time, left internal thoracic artery (LIMA) application, hospitalization time (P>0.05). The groups did not differ statistically in early or late mortality.
Full table
Clinical events: morbidity and mortality outcomes
Among 50 cases, 2 cases of each group died during in-hospital time (P>0.05). One ONCAB death was resulted from low cardiac output, renal dysfunction, ventricle fibrillation. Another died because of hypoxia, oliguria, deterioration of renal function. Though hematodialysis was administrated, patient’s unstable circulation led to death. Two OPCAB cases were resulted from malignant arrhythmia, low cardiac output syndrome. And the remaining 46 patients were cured and their cardiac functions were significantly improved (Table 1).
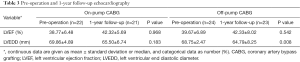
The mean follow-up time for ONCAB and OPCAB were (2.64±1.49) and (2.64±1.35) years. One-year follow-up echocardiographies were obtained in 1-year. At the 1-year follow-up, there was no significant difference between two revascularization strategies in LVEF and LVEDD (P>0.05). Albeit for each group, LVEF and LVEDD were slightly improved comparing to pre-procedure (Table 3).
Full table
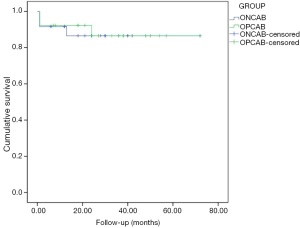
Kaplan-Meier analysis and event-free survival
One-year survival in ONCAB and OPCAB were 87.5% and 92.3% respectively (P>0.05). One year later, one mortality occurred in both group because of malignant arrhythmia and cardiac arrest. No significant differences were observed in the estimated survival of patients treated with ONCAB or OPCAB (Figure 1).
Discussion
Since the emerging of the OPCAB, many investigations have been carried out to compare the outcomes between OPCAB and ONCAB (8,9). Some studies suggest that OPCAB reduces cardiac complications and even benefit high-risk patients in regard to stroke prevention, less postoperative morbidity and mortality (5,10-12).
Cardioplegic arrest and CPB have been the mainstays of CABG surgery for almost 30 years. In this retrospective comparative study, patients with a number of common ‘high-risk’ co-morbidities-diabetes mellitus, renal insufficiency, giant left ventricle, poor LVEF were risky during operation. It would largely alleviate performer’s psychological pressure if we could achieve a stable hemodynamics by using CPB in such patients. Also, it was much more easier to exposure and sequence anastomosis. However, the theoretical and practical disadvantages of ONCAB have been widely described that it would trigger the diffuse systemic inflammatory response during and after cardiac surgery (13), platelet activation and changes to coagulation and fibrinolytic systems (14). Directly in touch with artificial surfaces of the extracorporeal circulation (ECC) induce a temporal change in patient’s immune system (15). Aortic manipulation, which used in conventional CABG, was a potential source of atheroemboli that could cause post-procedural cerebral infarction, especially for seriously aortic calcification patients. Comparing to OPCAB, ONCAB needs prolonged postoperative stay and occurred more postoperative complication such as renal impairment, coagulopathy, and even increased mortality (16-18). And this is consistent with our study. Comparing to OPCAB, there were significant higher rate of renal dysfunction, longer hospitalization in ONCAB.
The primary administration of OPCAB in early nineties was mainly to relatively low risk surgical patients (19). Since then, a large body of researches have conducted to suggest many potential advantages of the OPCAB technique over ONCAB technique in different group of high-risk patients (17,20,21). However, OPCAB requires much more manipulations of target coronary artery than arrested heart with CPB, such as shunt insertion, octopus stabilizer position. And it’s also a big challenge for surgeon to operate on a beating heart. Technically, it is easy to injury to the coronary endothelium and finally predispose the anastomosis to early failure from thrombosis or late failure from intimal hyperplasia (22). In our OPCAB experience, severely dilated left ventricle could make the surgery technically challenging, especially to procedure lateral wall grafting. What’s more, the giant left ventricle with compromised LVEF was more sensitive to a reduction in preload as was seen with right ventricular compression when exposing the grafting of lateral wall. So when anastomosing lateral wall grafting, attention was required to surgical details to maintain hemodynamic stability (23-25). It would be wise to open the right pleural space and removed the right pleuro-pericardial fat pad to rotate the heart into right chest cavity and avoid cardiac compression against the pericardium. Additionally, beta blockade and adenosine was given to slow the heart and facilitate placing difficult stitches. Hemodynamics tends to be more stable when the anterior vessels were grafted and perfused before approaching the posterolateral wall target. Moreover, it was safe and feasibly to position IABP before operation. The application of IABP permits patients to undergo CABG with lower perioperative myocardial infraction and mortality by stabling the haemodynamics during operation. In the diastolic phase of cardiac cycle, the balloon inflated, resulted in elevated coronary perfusion pressure, augmented coronary blood flow and increased myocardial oxygen supply. In the systolic phase of cardiac cycle, the balloon deflates rapidly, decrement the myocardial workload and oxygen demand. And it may explain why there were more IABP implication in OPCAB group. Additionally, CABG preserves already functioning muscle against further infarction and recruits hibernating muscle that leads to the objective improvement in ejection fraction and to the amelioration of congestive heart failure. Improvement in left ventricular function after CABG was objectively demonstrated. The mean ejection fraction was 38.77%±6.48% and 39.67%±6.89% respectively in ONCAB and OPCAB group before bypass grafting and 42.32%±5.69% and 42.33%±8.02% after 1-year follow up. There was no significant difference between ONCAB and OPCAB with respect to the 1-year mortality and 1-year graft occlusion. And this is consistent to a study that recent published on the New England Journal of Medicine (26).
Taken together, our study confirms that both strategies, ONCAB and OPCAB are suitable alternatives for patients with severely dilated. Moreover, OPCAB is associated with a reduction of renal dysfunction, operation duration and length of ventilation compared with patients undergoing ONCAB. However, OPCAB should be individualized for each single patient in the light of the comorbidities, life expectancy and surgeon’s dexterity.
Limitations of the study
There are some limitations to this research. Firstly, follow-up period is relatively short. So only 1-year follow-up echocardiography was analysed. A longer duration of follow-up may yield more results and it can help us further elucidate which procedure is much more suitable for giant left ventricle patient. Secondly, the relatively small sample size of our patients with severely dilated left ventricle limits conclusions that can be drawn regarding this subset of patients. Thirdly, it would be better if we conduct propensity match model in this study to eliminate some irrelevant factors.
Acknowledgements
We are grateful that Ruijin Hospital provides us a so awesome platform to carry out such interesting research.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Regional Ethics Committee of Shanghai Jiao Tong University and informed consents were obtained from all patients.
References
- Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1993;362:801-9. [Crossref] [PubMed]
- SoS Investigators. Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomised controlled trial. Lancet 2002;360:965-70. [Crossref] [PubMed]
- Puskas JD, Thourani VH, Kilgo P, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg 2009;88:1142-7. [Crossref] [PubMed]
- Magee MJ, Coombs LP, Peterson ED, et al. Patient selection and current practice strategy for off-pump coronary artery bypass surgery. Circulation 2003;108 Suppl 1:II9-14. [Crossref] [PubMed]
- Emmert MY, Salzberg SP, Theusinger OM, et al. Off-pump surgery for the poor ventricle? Heart Vessels 2012;27:258-64. [Crossref] [PubMed]
- Hlavicka J, Straka Z, Jelinek S, et al. Off-pump versus on-pump coronary artery bypass grafting surgery in high-risk patients: PRAGUE-6 trial at 30 days and 1 year. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2016;160:263-70. [Crossref] [PubMed]
- Yu L, Gu T, Shi E, et al. Off-pump versus on-pump coronary artery bypass surgery in patients with triple-vessel disease and enlarged ventricles. Ann Saudi Med 2014;34:222-8. [PubMed]
- Brinkman WT, Squiers JJ, Filardo G, et al. Perioperative Outcomes, Transfusion Requirements, and Inflammatory Response After Coronary Artery Bypass Grafting With Off-Pump, Mini-Extracorporeal, and On-Pump Circulation Techniques. J Investig Med 2015;63:916-20. [PubMed]
- Dhurandhar V, Saxena A, Parikh R, et al. Outcomes of On-Pump versus Off-Pump Coronary Artery Bypass Graft Surgery in the High Risk (AusSCORE > 5). Heart Lung Circ 2015;24:1216-24. [Crossref] [PubMed]
- Keeling WB, Williams ML, Slaughter MS, et al. Off-pump and on-pump coronary revascularization in patients with low ejection fraction: a report from the society of thoracic surgeons national database. Ann Thorac Surg 2013;96:83-8: discussion 88-9.
- Marui A, Okabayashi H, Komiya T, et al. Benefits of off-pump coronary artery bypass grafting in high-risk patients. Circulation 2012;126:S151-7. [Crossref] [PubMed]
- Afilalo J, Rasti M, Ohayon SM, et al. Off-pump vs. on-pump coronary artery bypass surgery: an updated meta-analysis and meta-regression of randomized trials. Eur Heart J 2012;33:1257-67. [Crossref] [PubMed]
- Yokoyama T, Baumgartner FJ, Gheissari A, et al. Off-pump versus on-pump coronary bypass in high-risk subgroups. Ann Thorac Surg 2000;70:1546-50. [Crossref] [PubMed]
- Vallely MP, Bannon PG, Bayfield MS, et al. Quantitative and temporal differences in coagulation, fibrinolysis and platelet activation after on-pump and off-pump coronary artery bypass surgery. Heart Lung Circ 2009;18:123-30. [Crossref] [PubMed]
- Fransen E, Maessen J, Dentener M, et al. Systemic inflammation present in patients undergoing CABG without extracorporeal circulation. Chest 1998;113:1290-5. [Crossref] [PubMed]
- Elahi MM, Yii M, Matata BM. Significance of oxidants and inflammatory mediators in blood of patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 2008;22:455-67. [Crossref] [PubMed]
- Bahar I, Akgul A, Ozatik MA, et al. Acute renal failure following open heart surgery: risk factors and prognosis. Perfusion 2005;20:317-22. [Crossref] [PubMed]
- Chertow GM, Levy EM, Hammermeister KE, et al. Independent association between acute renal failure and mortality following cardiac surgery. Am J Med 1998;104:343-8. [Crossref] [PubMed]
- Benetti FJ, Naselli G, Wood M, et al. Direct myocardial revascularization without extracorporeal circulation. Experience in 700 patients. Chest 1991;100:312-6. [Crossref] [PubMed]
- Emmert MY, Emmert LS, Martinez EC, et al. Off-pump coronary bypass surgery is safe in patients with a low ejection fraction (< or =25%). Heart Surg Forum 2010;13:E136-42. [Crossref] [PubMed]
- Litmathe J, Kurt M, Feindt P, et al. The impact of pre- and postoperative renal dysfunction on outcome of patients undergoing coronary artery bypass grafting (CABG). Thorac Cardiovasc Surg 2009;57:460-3. [Crossref] [PubMed]
- Hangler HB, Pfaller K, Ruttmann E, et al. Effects of intracoronary shunts on coronary endothelial coating in the human beating heart. Ann Thorac Surg 2004;77:776-80. [Crossref] [PubMed]
- Hart JC. Multivessel off-pump coronary bypass with the Octopus experience in 226 patients. J Card Surg 2000;15:266-70. [Crossref] [PubMed]
- Hart JC. Hemodynamic stability and lessons learned: a four-year OPCAB experience. Heart Surg Forum 2001;4:335-8. [PubMed]
- Hart JC, Puskas JD, Sabik JF 3rd. Off-pump coronary revascularization: current state of the art. Semin Thorac Cardiovasc Surg 2002;14:70-81. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013;368:1179-88. [Crossref] [PubMed]


