Blood loss in pelvic ring fractures: CT-based estimation
Introduction
Due to associated injuries and bleeding the mortality after pelvic ring fractures is up to 20% (1). Common sources of bleeding are arterial branches of the iliac vessels, the pre-sacral venous plexus and large cancellous bone surfaces. The assessment of the amount of primary blood loss is difficult and a review of literature reveals no clear standards (2). The fractures of the pelvic ring are classified in stable ring, partially stable ring and unstable ring fractures. The latter are divided in C1-C3 (for details see https://www2.aofoundation.org/wps/portal/surgery?showPage=diagnosis&bone=Pelvis&segment=Ring). In unstable pelvic ring fractures a blood loss of approximately 9 to 15 units of blood has to be expected whereas total blood loss is mainly evaluated retrospectively and indirectly (3). The acute total blood loss and hemodynamic status of the patient can be assessed by clinical shock signs. Most commonly systolic arterial blood pressure and haemoglobin concentration are utilized. These are however not precise and even in patients with low arterial blood pressure and pelvic fractures no correlation was found to the outcome (4). Further diagnostic possibilities are ultrasound, computed tomography and angiography which allowed an estimation of the amount of blood loss but the exact volume cannot be calculated without further reconstruction (5). The aim of the current study was to perform a CT-based estimation of blood loss at an early stage after pelvic ring fractures to correlate these results to the mortality.
Methods
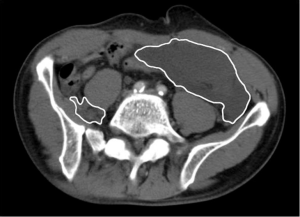
Between 2008 and 2011, 97 patients with AO/OTA C-type pelvic ring fractures were identified at our hospital. Inclusion criteria were patients above the age of 18, primary care at our hospital, AO/OTA C-type pelvic ring fracture and CT diagnostics within 2 hours of the initial trauma. Exclusion criteria were patients above the age of 65, pre-existing coagulation disorders, medication with an influence on coagulation and pre-existing disorders influencing bone metabolism. The inclusion criteria were met by 42 patients. All patients were hemodynamically stable at the time of admission and received CT poly-trauma scans (Brilliance 64 slice scanner; Philips Healthcare; Hamburg, Germany; 1 mm slice thickness) with intravenous contrast (Imeron 400, Bracco Imaging; Konstanz, Germany) within 2 hours of the initial trauma. The patients were divided into three groups based on their AO/OTA C-type fracture sub-classification. CT data was analysed with the Osirix DICOM viewer (Version 5.8; Pixmea; Geneva, Switzerland). Manual volumetric CT was performed. In the portal venous CT phase the bleeding region of interest (ROI, cm2) was marked slice by slice (Figure 1). Calculation of the intramuscular, interstitial and total blood volume was then performed with the Osirix software by two senior researchers. Statistical analysis was performed with Graph Pad Prism (Version 6.0; GraphPad Software Inc.; La Jolla CA, USA). Normal distribution was tested with the Shapiro Wilk test. Analysis of variance with a Bonferroni post-test, Kruskal Wallis test and Pearson correlation analysis were performed. P<0.05 was defined as statistically significant. The study was approved by the local ethics committee.
Results
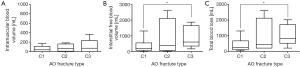
In all, 42 patients met the inclusion and exclusion criteria. The average patient age was 47 years ±19; 60% were female. The most common trauma mechanisms were car accidents (55%), falls from a height of over 3 meters (33%) and falls from less than 3 meters (14%). Of the patients 29 had an AO/OTA C1-type injury, 4 a C2-type injury and 9 a C3-type injury. The average time from admission to completed CT scan was 26±18 minutes. No significant difference in scan time was seen between all three groups. Overall mortality was 12%. Higher early total blood loss significantly correlated to mortality [rp=0.55; P<0.001; f(x) =1,374.0±531.9] and, generally, significantly higher blood losses were encountered in deceased patients (1,906±549 vs. 541±567 mL; P<0001). The severity of injuries might be comparable because the Injury Severity Score (ISS) did not differ significantly. There were no obvious other injuries or bleeding causes in the investigated patients but those cannot be completely excluded. No significant difference between the various AO/OTA C-type fractures was seen with regard to hemoglobin concentration (C1-type: 11.3±2.4 g/dL; C2-type: 11.2±1.5 g/dL; C3-type: 10.1±2.3 g/dL), ISS (27.3±10.4; 32.0±6.5; 32.6±10.8) or systolic blood pressure (116±29 mmHg; 103±25 mmHg; 91±13 mmHg). Based on the AO/OTA C type classification of the pelvic ring fractures significant differences in interstitial (392±502 vs. 888±663 mL; P<0.05) and total blood loss (476±535 vs. 1,005±649 mL; P<0.05) were seen in the comparison of C1- and C3-type fractures. There was no significant difference in intramuscular blood loss (C1-type: 84±153 mL; C2-type: 77±81 mL; C3-type: 117±134 mL) in any of the fracture types. The average total blood loss after C1-type fractures was 476 mL, after C2-type fractures 931 and 1,005 mL after C3-type fractures (Figure 2).
Discussion
Dienstknecht et al. showed that patients with combined anterior/posterior pelvic ring fractures had a poor outcome (6). Among other reasons this fact might be caused by a high, early blood loss. Holstein et al. were able to show that more than 60% of the deaths after pelvic ring fractures can be attributed to excessive blood loss (7). This is in accordance with our results, where higher early bleeding volumes correlated to increased mortality. The volumetric CT analysis requires up to 20 minutes. Therefore, this parameter is difficult to include in the early clinical management. To include the volumetric CT in therapeutic algorithms this procedure should be significantly shortened. The contrast differences required differentiating between blood and surrounding tissues are also given in pelvic scans. An association of fracture dislocation at the pubic symphysis and obturator ring with the amount of blood loss in conventional X-ray studies has been shown (8). However, information about fracture diastases can be lost on emergency X-rays if appropriate compression therapy with pelvic binders has been applied. To our knowledge, no correlating assessment of the association between blood loss and AO/OTA fracture types and related mortality has yet been carried out. Our results show a significant increase in interstitial blood volume and total blood volume lost for AO/OTA C3-type fractures in comparison with C1-type fractures during the first two hours after trauma. Based on the classification alone, the expected blood loss in initially hemodynamically stable patients can be predicted. This classification can be rapidly applied from native CT data during the early care of poly-trauma patients if appropriate care protocols exist (9,10). Trauma severity, decreased haemoglobin concentration and low blood pressure all indicated slight tendencies towards worse fracture types, but differences between the three fractures groups did not prove statistically significant. These early and low volume blood losses are however important predictors of the overall outcome, since they significantly correlated to higher mortalities, as seen in our results. Early prediction of a higher expected blood loss could lead to an earlier adaptation of volume resuscitation, possibly decreasing the shock severity and overall mortality (10). Our results are limited by low patient numbers in the group of AO/OTA C2-type fractures. Large-scale studies with a higher patient number especially in this group are needed to further investigate the influence of this fracture type on blood loss. However, the significant difference between C1 and C3-type fractures is sufficiently substantiated.
Conclusions
The CT-based estimation of early blood loss is correlated to mortality. Furthermore, based on the AO/OTA sub-classification of C-type fractures a prediction of the early blood is possible.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the local ethics committee (1622601). All patients of the Saarland University Hospital have given their consent for publication of anonymized clinical data.
References
- Hauschild O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic fractures: results from the German pelvic injury register. J Trauma 2008;64:449-55. [Crossref] [PubMed]
- Tosounidis TI, Giannoudis PV. Pelvic fractures presenting with haemodynamic instability: treatment options and outcomes. Surgeon 2013;11:344-51. [Crossref] [PubMed]
- Ruatti S, Guillot S, Brun J, et al. Which pelvic ring fractures are potentially lethal? Injury 2015;46:1059-63. [Crossref] [PubMed]
- Ojodu I, Pohlemann T, Hopp S, et al. Predictors of mortality for complex fractures of the pelvic ring in the elderly: a twelve-year review from a German level I trauma center. Injury 2015;46:1996-8. [Crossref] [PubMed]
- Brun J, Guillot S, Bouzat P, et al. Detecting active pelvic arterial haemorrhage on admission following serious pelvic fracture in multiple trauma patients. Injury 2014;45:101-6. [Crossref] [PubMed]
- Dienstknecht T, Pfeifer R, Horst K, et al. The long-term clinical outcome after pelvic ring injuries. Bone Joint J 2013;95-B:548-53. [Crossref] [PubMed]
- Holstein JH, Culemann U, Pohlemann T, et al. What are predictors of mortality in patients with pelvic fractures? Clin Orthop Relat Res 2012;470:2090-7. [Crossref] [PubMed]
- Blackmore CC, Cummings P, Jurkovich GJ, et al. Predicting major hemorrhage in patients with pelvic fracture. J Trauma 2006;61:346-52. [Crossref] [PubMed]
- Scolaro JA, Wilson DJ, Routt ML, et al. Use of the initial trauma CT scan to aid in diagnosis of open pelvic fractures. Injury 2015;46:1999-2002. [Crossref] [PubMed]
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013;39:165-228. [Crossref] [PubMed]


