Mitral valve repair with the “respect” approach in dialysis-dependent patients: a single-center experience
Introduction
The prevalence of end-stage renal disease (ESRD) is increasing and greater numbers of dialysis-dependent patients are undergoing mitral valve surgery because of mitral regurgitation. Despite recent advances in perioperative cardiovascular care, significant challenges remain and outcomes are unsatisfactory (1,2). Although mitral valve repair is associated with significantly better survival than mitral valve replacement, dialysis patients still undergo mitral valve repair less frequently than non-dialysis patients, and surgical selection in these patients is based on limited data (3).
Prolapse of the posterior leaflet is the most frequent dysfunction of a degenerative mitral valve, and is the first lesion accessible for repair. Mitral valve repair with the “respect” approach was first introduced by Perier et al. (4), followed by modified techniques (5,6), and several studies have shown that the “respect” approach can correct the prolapse without leaflet resection and can transform the prolapsed leaflet into a smooth and vertical buttress ensuring the best coaptation surface (7,8).
We retrospectively reviewed the clinical data of dialysis-dependent patients undergoing mitral valve repair with the “respect” approach between 2012 and 2015 and evaluated the results.
Methods
Between 2012 and 2015, five dialysis-dependent patients with severe mitral regurgitation resulting from prolapse of the posterior leaflet underwent mitral valve repair with the “respect” approach in our institution. We retrospectively reviewed patients’ clinical data. The group included three males and two females with a mean age of 54.6±5.2 years (range, 47–62 years). Preoperatively, one patient was in New York Heart Association class II, and four patients were in class III. Concomitant cardiac diseases included tricuspid valve regurgitation in three patients and none had previously undergone cardiac surgery or thoracic injury. Patients’ clinical profiles are presented in Table 1.
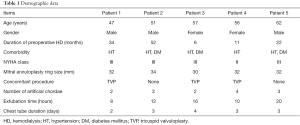
Full table
This study was retrospectively approved by the ethics committee of our institution (LS 1611), which waived the need to obtain patient consent.
Operative approach
Operations were performed with cardiopulmonary bypass and mild systemic hypothermia. Myocardial protection was achieved with tepid blood cardioplegia, and mitral valve repair was performed according to previously described techniques (9). Briefly, a CV-4 expanded polytetrafluoroethylene (Gore-Tex; W. L. Gore & Associates, Flagstaff, AZ, USA) suture was used to resuspend the free edge of the prolapsed leaflet. The number and placement of the artificial chordae may vary according to the extent and location of the prolapsed area; however, the basic architecture of the subvalvular apparatus must be respected.
Mitral ring annuloplasty was performed routinely in all patients with a Carpentier-Edwards Physio ring (model 4450; Edwards Lifesciences, Irvine, CA, USA). The size of the ring was selected according to the standard criteria: intertrigonal distance and the anterior leaflet surface area. After separation from cardiopulmonary bypass, the repair was evaluated by transesophageal echocardiography. In three patients requiring tricuspid repair, a Carpentier-Edwards annuloplasty ring (Edwards Lifesciences) was also used.
Perioperative management
Patients were thoroughly evaluated preoperatively, including by coronary angiography. Anemia and hypoproteinemia were eliminated by transfusion of red blood cells or human serum albumin, and antibiotics were used in cases of infection including bronchitis or oral infections.
Patients underwent hemodialysis (HD) the day before the operation, and ultrafiltration during cardiopulmonary bypass was also routinely used. On postoperative 1 day, heparin-free continuous veno-venous hyperfiltration-dialysis was adopted to maintain water balance and avoid bleeding complication. Conventional HD was resumed 3–6 days postoperatively once heart function stabilized.
Oral anticoagulation therapy (coumarin) began 1 day postoperatively with a target international normalized ratio of 2.5. After 3 months, anticoagulant treatment was discontinued at the discretion of the referring physician, provided the patient was in sinus rhythm (10).
Statistical analysis
Computerized statistical analysis of the data was performed using SPSS 19.0 software (IBM Corp., Armonk, NY, USA). Descriptive statistics are reported as the mean ± standard deviation for continuous variables and as frequencies and percentages for categorical variables unless otherwise noted. Comparisons between groups were made using unpaired t-tests for continuous variables.
Results
All five patients survived and all patients’ data were retrospectively evaluated in the final analysis. Cardiopulmonary bypass times and aortic cross-clamp times were 82.4±16.8 and 68.3±20.2 minutes, respectively. The final follow-up was completed in April 2016 through telephone contact with patients or their referring physicians. Follow-up ranged from 3–48 months with a median of 24±8.9 months. No patients were lost to follow-up.
Patients’ cardiac function improved post-operatively with two patients in New York Heart Association class I and three patients in class II. There was no or trivial mitral valve regurgitation in three patients, mild regurgitation in two, and moderate regurgitation or above in none. Left ventricular end diastolic volume decreased significantly from 166.2±32.7 mL preoperatively to 123.1±24.5 mL postoperatively (P<0.001).
Discussion
Although mitral valve repair has gained increasing acceptance as the procedure of choice for correction of mitral regurgitation following prolapse (11), the superiority of mitral valve repair over replacement among ESRD patients has not been well-established. Several recent studies have shown that mitral valve repair with the “respect” approach can correct the prolapse without leaflet resection and with excellent results; however, there is little information regarding this technique in ESRD patients.
In our study, we adopted the “respect” approach to treat dialysis patients with posterior leaflet prolapse. Implantation of artificial chordae and rings instead of a prosthetic valve avoided the complications associated with prosthetic valves.
We successfully used the “respect” technique in five patients on chronic dialysis. During follow-up, no patients underwent reoperation or experienced severe cardiac-associated complications. Heart function greatly improved and left ventricular end-diastolic volume decreased significantly. Considering the ideal mitral valve surgery for dialysis patients, we adopted mitral valve repair rather than replacement, which provided good hemodynamics to prevent heart failure; avoided postoperative warfarin, which prevented bleeding and thromboembolic complications; and avoided foreign body implantation, which kept the risk of infection as low as possible.
Patients on chronic dialysis exhibit an immune defect characterized by an increased susceptibility to infections and a decreased immune response; therefore, there is a higher risk for infectious complications in these patients (12). We carefully evaluated our patients, and antibiotics were used routinely to treat infections preoperatively. Postoperatively, antibiotics were used routinely to avoid infections, and extubation occurred as early as possible to decrease respiratory infection risk.
Intraoperative transesophageal echocardiography (TEE) played an important role in the surgical planning and postoperative evaluation of mitral valve repair in our patients. Mitral valve pathologies were carefully evaluated preoperatively to verify the lesion location, and we excluded patients with anterior leaflet or bi-leaflet prolapse because these repair operations are more demanding and require more time. Postoperative results were also evaluated by TEE and reoperation was quickly performed to address significant mitral regurgitation.
Timing the reintroduction of HD postoperatively was critical. Usually, patients underwent HD the day before the operation, and ultrafiltration was routinely used during cardiopulmonary bypass; therefore, we avoided HD on the day of operation to avoid bleeding complications without fear of fluid overload. Patients underwent heparin-free continuous veno-venous hyperfiltration-dialysis to maintain the stability of the internal environment on postoperative day 1, and resumed standard HD with heparin 3–6 days postoperatively when heart function stabilized.
Conclusions
Based on our very limited experience, we advocate mitral valve repair with the “respect” approach in dialysis-dependent patients with prolapse of the posterior leaflet. This technique provides good and stable results with appropriate perioperative management. Although longer term follow-up in a larger population is necessary, the “respect” approach may allow new strategies in dialysis-dependent patients undergoing mitral valve repair, avoiding the bleeding and thromboembolic complications that result from oral anticoagulant agents.
Acknowledgements
Funding: This work is supported by Science and Technology Commission of Shanghai Municipality of China (11ZR1422500). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was retrospectively approved by the ethics committee of our institution (LS 1611), which waived the need to obtain patient consent.
References
- Phan K, Zhao DF, Zhou JJ, et al. Bioprosthetic versus mechanical prostheses for valve replacement in end-stage renal disease patients: systematic review and meta-analysis. J Thorac Dis 2016;8:769-77. [Crossref] [PubMed]
- Takeda K, Miyata H, Motomura N, et al. Contemporary perioperative results of heart valve replacement in dialysis patients: analysis of 1,616 patients from the Japan adult cardiovascular surgery database. J Heart Valve Dis 2013;22:850-8. [PubMed]
- Vassileva CM, Brennan JM, Gammie JS, et al. Mitral procedure selection in patients on dialysis: does mitral repair influence outcomes? J Thorac Cardiovasc Surg 2014;148:144-150.e1. [Crossref] [PubMed]
- Perier P, Hohenberger W, Lakew F, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the "respect rather than resect" approach. Ann Thorac Surg 2008;86:718-25; discussion 718-25. [Crossref] [PubMed]
- Seeburger J, Noack T, Winkfein M, et al. Loop technique. Multimed Man Cardiothorac Surg 2010;2010:mmcts.2010.004523.
- Okamoto K, Yozu R, Kudo M. Loop-in-loop technique in mitral valve repair via minithoracotomy. Ann Thorac Surg 2012;93:1329-30. [Crossref] [PubMed]
- Perier P, Hohenberger W, Lakew F, et al. Minimally invasive repair of posterior leaflet mitral valve prolapse with the "respect" approach. Ann Cardiothorac Surg 2013;2:833-8. [PubMed]
- Perier P, Hohenberger W, Lakew F, et al. Prolapse of the posterior leaflet: resect or respect. Ann Cardiothorac Surg 2015;4:273-7. [PubMed]
- Salvador L, Mirone S, Bianchini R, et al. A 20-year experience with mitral valve repair with artificial chordae in 608 patients. J Thorac Cardiovasc Surg 2008;135:1280-7. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2014;148:e1-e132. [Crossref] [PubMed]
- Oliveira JM, Antunes MJ. Mitral valve repair: better than replacement. Heart 2006;92:275-81. [Crossref] [PubMed]
- Yamauchi T, Miyata H, Sakaguchi T, et al. Coronary artery bypass grafting in hemodialysis-dependent patients: analysis of Japan Adult Cardiovascular Surgery Database. Circ J 2012;76:1115-20. [Crossref] [PubMed]


