Predictive significance of detectable cardiac troponin I measured with a contemporary-sensitive assay in a real life experience
Introduction
Acute chest pain is one of the most common complaints leading patients to the emergency department (ED), accounting for up to 10% of all visits (1). Despite remarkable advances occurred in the past decades, the diagnosis, risk stratification and management of patients with chest pain continue to be challenging for the Emergency Physicians (EPs) (2). The thoughtful evaluation of suspected cases requires a high index of suspicion for acute coronary syndrome (ACS), but the EPs should also consider the kaleidoscope of frequently subtle and atypical presentations of ischemic heart disease, especially in certain patient populations such as in the elderly (3,4).
Chest pain can be due to a broad spectrum of conditions, ranging from totally harmless to severe and immediately life-threatening diseases. Amongst the latter, ACS (defined as a spectrum of disease ranging from unstable angina to myocardial infarction), pulmonary embolism, aortic dissection, tension pneumothorax, pericardial tamponade and esophageal rupture are the bogeyman of the EPs, who have the compelling need and duty to rule out potentially life-threatening causes and establish a diagnostic and management strategy which would allow a rapid and safe patient disposition (5). ACS, however, is the final diagnosis in only 20–25% of chest pain patients visited in ED (6), as well as in 45% of those admitted to a Chest Pain Unit (7).
In the last decades several studies reported a concerning high rate (between 2–4%) of patients discharged from the ED with missed ACS (8,9), also demonstrating that patients incorrectly discharged have a higher rate of short-term mortality, between 10–25%.
As for any other diagnostic area, biomarker testing has played a crucial role in the evaluation of patients with acute chest pain, even for prognostication of patients with ischemic heart disease (10). The World Health Organization (WHO) has played a major role in the formulation of diagnostic criteria for acute myocardial infarction (AMI) since the early 1970s. The first document, conventionally known as “European Myocardial Infarction registry criteria”, was published in 1976. At that time the diagnosis of AMI required suggestive findings emerging from the clinical history, electrocardiography (ECG), measurement of “cardiac enzymes” and, eventually, postmortem findings (11).
From the last decade of the past century, the introduction of tests for cardiac troponins (cTn), both I (cTnI) and T (cTnT), has substantially reduced the likelihood of erroneously discharge of patients with ACS, but still some doubts persist about their optimal clinical use in short stay units such as the ED (12,13). Many still believe that the contemporary cTn assays may not be characterized by optimal precision at the recommended 99th percentile threshold value compared to the emerging high-sensitivity (HS) techniques. Therefore, ED physicians are often still reluctant to discharge patients without ordering additional tests (i.e., imaging or stress test), despite the use of serial testing may ultimately improve the diagnostic sensitivity and the negative predictive value (NPV) (14). The development of a new generation of HS-cTn immunoassays has hence represented a paradigm shift, since these methods may be able to identify minor increases of cTn concentration at an earlier stage after the onset of chest pain and, most notably, shortening the timing of serial sampling (15).
Although a number of diagnostic algorithms have been developed and used so far, mainly designed for rapid ruling-in or ruling-out ACS in patients with chest pain, a definitive and universally agreed strategy is still far from being identified and universally acknowledged (16).
In our hospital, a contemporary-sensitive cTnI immunoassay (AccuTnI, Beckman Coulter, Brea, CA, USA) has been in use since the 2005. This method allows a reliable measurement of troponin levels in the range comprised between 0.01–100 ng/mL, with a limit of detection of 0.01 ng/mL (17). Until the year 2014 the upper reference limit (URL) corresponding to the 99th percentile was 0.05 ng/mL. The publication of a subsequent study by Zaninotto et al. (18) has allowed to revised the decision limit, demonstrating that the optimal diagnostic threshold (i.e., the value with 10% imprecision) was 0.034 ng/dL, thus persuading the manufacturer to recommend lowering the diagnostic threshold to 0.035 ng/mL in the year 2014. Due to recent data, mostly emerging from studies using HS immunoassays and pinpointing that cTn values below the conventional cut-offs may still retain clinical value for diagnosis and prognostication of chest pain patients, we planned a study to evaluate the predictive significance of cTnI values comprised between the limit of detection of the method and the 99th percentile in all consecutive patients evaluated for a suspected ACS in the ED.
Methods
All the records of patients for whom at least one cTnI measurement was ordered by the EP have been retrieved from the electronic hospital database during a period of 181 days (1st January to 30th June, 2014). The University Hospital of Parma is a 1,150-bed teaching general hospital, serving a population of about 435,000, and is the only hospital in the area. This hospital is a level 2 Trauma Center and a referral center for stroke and cases of AMI. All consecutive patients for whom a cTnI was ordered for ruling in or ruling out an ACS during the first semester of the year 2014 have hence been considered.
Inclusion criteria were age ≥18 years and availability of cTnI values (AccuTnI, Beckman Coulter) comprised between 0.01 ng/mL (i.e., the limit of detection of the assay) (17) and 0.05 ng/mL, as obtained in samples collected at three time point (i.e., at admission, and 3 and 6 hours thereafter). Exclusion criteria were undetectable cTnI values (i.e., <0.01 ng/mL) in all samples, cTnI values >0.05 ng/mL in at least one of the samples collected during serial sampling, or a final diagnosis of ST-elevation myocardial infarction (STEMI) in the ED.
The population sample was than divided in three main groups: (I) patients discharged from the ED; (II) patients admitted to the ED for diagnostic uncertainty or comorbidities; (III) patients who died in the ED. Amongst the former two groups, the data of all patients with following admissions to the ED within 30 days after earlier discharge were carefully analyzed, with particular focus on a diagnosis of ACS during the second visit. The laboratory and clinical information of patients who were admitted to the hospital was also analyzed, in order to identify possible development of ACS during the hospital stay.
Results
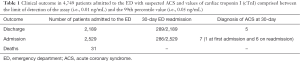
A total of 4,749 patients with a cTnI value comprised between 0.01–0.05 ng/mL were identified among 57,879 ED visits throughout the study period. Overall, 2,189 patients (46.1%) were directly discharged from the ED, 2,529 (53.25%) were admitted to the hospital and 31 (0.65%) died during permanence in the ED.
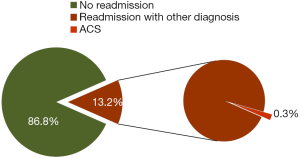
A total number of 289 patients out of the 2,189 who were discharged (i.e., 13.2%) had an additional ED visit within 30 days (Table 1). Five out of 289 (i.e., 0.23% of the whole sample, and 1.7% of those with a second attendance) had a diagnosis of ACS on the second visit. One additional patient with ACS was excluded, since he developed a heart attack probably due to withdrawing dual antiplatelet therapy (i.e. aspirin and clopidogrel) before a surgical intervention.
Full table
Only one of the 2,529 patients admitted to the hospital (i.e., 0.04%) developed an ACS during hospital stay. In this case, however, the second and third cTnI values were considerably increased, showing a typical incremental trend in the medical ward. As such, this ACS case cannot be classified as a “missed diagnosis”, but simply as an evolving myocardial ischemia started during the permanence in the ED and definitely evolved in the ward.
Considering the admitted patients, six patients amongst the 286 cases with an additional ED admission within 30 days from the first ED visit were diagnosed with an ACS during the second visit (Table 1). These hence represented 0.2% of the overall number of patients discharged (NPV of AccuTnI, 0.997; 95% CI, 0.994–0.999), and 2.1% of those with a second admission (NPV of AccuTnI, 0.979; 95% CI, 0.955–0.992) (Figure 1).
None of the patients with an ACS diagnosis on the second ED visit had a single diagnostic cTnI value (i.e., >0.05 ng/mL) during the first ED evaluation. Even more importantly, none of these patients also had a cTnI concentration higher than the value with 10% imprecision (i.e., >0.035 ng/mL). It is also noteworthy that none of these ACS patients had undetectable cTnI values in all samples collected during the former ED evaluation. However, they all had well recognized cardiovascular risk factors. One patient, with a cTnI value of 0.01 ng/mL during the first admission, presented with highly suggestive symptoms (typical chest pain accompanied by dyspnea) and voluntarily left the ED against EP recommendation, thus missing the possibility of performing additional investigations. Another patient was readmitted approximately 48 hours after ED discharge and was finally diagnosed with an ACS despite negative stress test ECG and non-diagnostic cTnI values during the former admission.
The thoughtful analysis of cTnI values of these patients also revealed that in ten of them (90.9%) cTnI was <0.035 ng/mL. The only patient showing a cTnI value comprised between 0.035–0.05 ng/mL (i.e., 0.04 ng/mL, a value between the formerly accepted cut-off and the 10% imprecision threshold) was admitted with a diagnosis of heart failure and no further testing was performed in the ED. However, a typical cTnI kinetics suggestive for ACS developed during the hospital stay, thus meaning that the patients was misdiagnosed and classified as having a very low risk of myocardial ischemia according to the initial clinical assessment by the EP. It should hence be considered a clinical and not an analytical problem.
Discussion
The results of our study suggest that the use of a contemporary-sensitive cTnI immunoassay combined with clinical judgment and ECG still represents a reliable strategy for ruling in and ruling out ACS in patients admitted to the ED. Interestingly, we could also confirm that the value of cTnI (both the 99th percentile or the value with 10% imprecision) measured with a contemporary-sensitive method has a very high NPV at 30 days (i.e., between 0.979 and 0.997), thus practically reproducing previous data published in studies using HS immunoassays.
The number of HS immunoassays for measuring both cTnI and cTnT is rapidly and constantly increasing, based on the assumption that these methods are analytically superior and may hence allow to accelerate the diagnostic evaluation of patients with suspected ACS, especially using rapid rule-in and rule-out protocols (19,20). Nevertheless, some questions remains. First, the time between the onset of symptoms and ED presentation of patients with ACS often exceeds 1–2 hours in the real practice, thus considerably weakening the potential advantage of early diagnoses allowed by HS immunoassays. This is indeed a critical issue, because it may generate serious harm to the patients (21). Then, despite the current goal for the turnaround time (TAT) of cTn testing is 60 minutes, this expectation cannot be really met in many health care facilities. This is mostly due to various factors such as the distance between the ED and the laboratory, the time needed for preanalytical processing of the samples (especially for check-in and centrifugation in stat laboratories managing hundreds of specimens at the same time), the time needed for sample analysis (usually comprised between 15–25 min) and results validation, as well as the gap between digital transmission of data and reading and interpretation by the EPs who work in increasingly overcrowded EDs. Therefore, the main strength of HS-cTn immunoassays, which is represented by the possibility to use much shorter sampling protocols, may be ultimately frustrated in real life scenarios (22). Last but not least, the presence of increasing (or decreasing) cTn values is mandatory according to all available recommendations for diagnosing ACS, but in many cases short intervals of testing (i.e., 1 hour) do not allow to define a kinetics suggestive enough for the final diagnosis of myocardial ischemia (21,23).
It is also noteworthy that a recent study in a cohort of 2100 patients presenting to the ED who had cTnI tested at 0, 3, 6 and 9 hours with two different assay (i.e., a contemporary-sensitive and HS immunoassays), showed that the overall proportion of patients with cTnI concentrations above the 99th percentile was not significantly different between the methods (i.e., 31% with the contemporary-sensitive immunoassay and 26% with the HS technique) (24). Unfortunately, the Authors did not provide any clinical data about the patients, thus making impossible to correlate their findings with outcomes, as in our study.
Conclusions
The results of our retrospective study seemingly provide reliable evidence that the use of a contemporary-sensitive cTnI immunoassay in the context of an appropriate diagnostic protocol (i.e., sampling time at ED admission and 3 and 6 hours afterwards), represents a safe and effective strategy for ruling in and ruling out ACS in patients presenting to the ED, exhibiting a NPV as high as 0.997. Additional research is hence needed to establish whether the new generation of HS-cTn immunoassays may definitely outstrip more conventional methods in the clinical practice of an overcrowded ED for diagnosing ACS, as well as for stratifying the future risk of myocardial ischemia (25).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective observational study was carried in accordance with the Declaration of Helsinki and under the terms of relevant local legislation.
References
- Mockel M, Searle J, Muller R, et al. Chief complaints in medical emergencies: do they relate to underlying disease and outcome? The Charité Emergency Medicine Study (CHARITEM). Eur J Emerg Med 2013;20:103-8. [Crossref] [PubMed]
- Lippi G, Cervellin G. Acute coronary syndrome: many doubts, some answers. Ann Transl Med 2016;4:187. [Crossref] [PubMed]
- Cervellin G, Rastelli G. The clinics of acute coronary syndrome. Ann Transl Med 2016;4:191. [Crossref] [PubMed]
- Lippi G, Sanchis-Gomar F, Cervellin G. Chest pain, dyspnea and other symptoms in patients with type 1 and 2 myocardial infarction. A literature review. Int J Cardiol 2016;215:20-2. [Crossref] [PubMed]
- Fruergaard P, Launbjerg J, Hesse B, et al. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. Eur Heart J 1996;17:1028-34. [Crossref] [PubMed]
- Goodacre S, Cross E, Arnold J, et al. The health care burden of acute chest pain. Heart 2005;91:229-30. [Crossref] [PubMed]
- Conti A, Paladini B, Toccafondi S, et al. Effectiveness of a multidisciplinary chest pain unit for the assessment of coronary syndromes and risk stratification in the Florence area. Am Heart J 2002;144:630-5. [Crossref] [PubMed]
- Pope JH, Aufderheide TP, Ruthazer R, et al. Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 2000;342:1163-70. [Crossref] [PubMed]
- McCarthy BD, Beshansky JR, D'Agostino RB, et al. Missed diagnoses of acute myocardial infarction in the emergency department: results from a multicenter study. Ann Emerg Med 1993;22:579-82. [Crossref] [PubMed]
- Lippi G, Franchini M, Cervellin G. Diagnosis and management of ischemic heart disease. Semin Thromb Hemost 2013;39:202-13. [Crossref] [PubMed]
- Cervellin G, Lippi G. Of MIs and men--a historical perspective on the diagnostics of acute myocardial infarction. Semin Thromb Hemost 2014;40:535-43. [Crossref] [PubMed]
- Casagranda I, Cavazza M, Clerico A, et al. Proposal for the use in emergency departments of cardiac troponins measured with the latest generation methods in patients with suspected acute coronary syndrome without persistent ST-segment elevation. Clin Chem Lab Med 2013;51:1727-37. [Crossref] [PubMed]
- Lippi G, Montagnana M, Aloe R, et al. Highly sensitive troponin immunoassays: navigating between the scylla and charybdis. Adv Clin Chem 2012;58:1-29. [Crossref] [PubMed]
- Smulders MW, Kietselaer BL, Schalla S, et al. Acute chest pain in the high-sensitivity cardiac troponin era: A changing role for noninvasive imaging? Am Heart J 2016;177:102-11. [Crossref] [PubMed]
- Lippi G. Biomarkers: Novel troponin immunoassay for early ACS rule-out. Nat Rev Cardiol 2016;13:9-10. [Crossref] [PubMed]
- Cervellin G, Mattiuzzi C, Bovo C, et al. Diagnostic algorithms for acute coronary syndrome-is one better than another? Ann Transl Med 2016;4:193. [Crossref] [PubMed]
- Lippi G, Dipalo M, Avanzini P, et al. Analytical assessment of the Beckman Coulter Unicel DxI AccuTnI+3 immunoassay. Diagnosis 2014;1:193-5. [Crossref]
- Zaninotto M, Mion MM, Novello E, et al. Precision performance at low levels and 99th percentile concentration of the Access AccuTnl assay on two different platforms. Clin Chem Lab Med 2009;47:367-71. [Crossref] [PubMed]
- Sandoval Y, Smith SW, Apple FS. Present and Future of Cardiac Troponin in Clinical Practice: A Paradigm Shift to High-Sensitivity Assays. Am J Med 2016;129:354-65. [Crossref] [PubMed]
- Mokhtari A, Borna C, Gilje P, et al. A 1-h Combination Algorithm Allows Fast Rule-Out and Rule-In of Major Adverse Cardiac Events. J Am Coll Cardiol 2016;67:1531-40. [Crossref] [PubMed]
- Jaffe AS. TRAPID or Trapped? Ann Emerg Med 2016;68:88-91. [Crossref] [PubMed]
- Lippi G, Cervellin G. Letter by Lippi and Cervellin regarding article, "High-sensitivity cardiac troponin in the distinction of acute myocardial infarction from acute cardiac noncoronary artery disease Circulation 2013;127:e353. [Crossref] [PubMed]
- Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33:2551-67. [Crossref] [PubMed]
- Love SA, Sandoval Y, Smith SW, et al. Incidence of Undetectable, Measurable, and Increased Cardiac Troponin I Concentrations Above the 99th Percentile Using a High-Sensitivity vs a Contemporary Assay in Patients Presenting to the Emergency Department. Clin Chem 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Lippi G, Cervellin G. The latest generation of troponin immunoassays: the "cholesterol" of the third millennium? J Am Coll Cardiol 2014;63:2883-4. [Crossref] [PubMed]


