Injury patterns in patients presenting with a recurrent anterior cruciate ligament tear following primary reconstruction
Introduction
Anterior cruciate ligament (ACL) injuries are amongst the most common sporting injuries to the knee (1,2). Injuries to the ACL often result in joint effusion, muscle weakness, altered movement and reduced functional performance (2). Anterior cruciate ligament reconstruction (ACLR) continues to be the mainstay of treatment for athletes who intend to return to sport (2). However, post-reconstruction outcomes are widely varied and poorer than previously reported (2-5). For athletes who return to sport, it is estimated that 1 in 4 will sustain a second knee injury (2).
Several studies in the literature have reported a higher rate of subsequent ACL injury following primary ACLR (1,6-8). These reports suggest that the incidence of ACL injury in the contralateral knee following primary ACLR of the ipsilateral knee is higher than the rate of graft rupture (6,8-10). Despite this, the etiology of the increased risk of ACL injuries of the contralateral knee as compared to the initially injured knee following primary ACLR is unknown. Risk factors such as notch width, knee alignment, deconditioning of the contralateral knee, and/or genetic predisposition have been postulated but unsubstantiated (10-13).
In addition, few studies have reported the incidence and patterns of concomitant knee injuries following the second ACL injury. This is primarily because studies that investigate the incidence and patterns of second ACL injuries exclude patients with concomitant meniscal and/or chondral pathologies (10,14-16).
Hence, the purpose of our present study was to describe the epidemiology of patients with a graft rupture following primary ACLR or a primary rupture of the contralateral ACL following primary ACLR of the ipsilateral knee. We aimed to compare the two groups of patients in terms of demographics, pre-injury level of sporting activity, mechanism of injury and time lapse between the first and second ACL injury and report the pattern and incidence of concomitant meniscal injuries.
Methods
We retrospectively reviewed the medical records of 42 patients who underwent a second ACLR between 2008 and 2013 by the senior author of the study. All patients who had an intra-operative diagnosis of graft rupture following a previous primary ACLR and/or an ACL injury of the contralateral knee following previous ipsilateral were included in this study. Patients who suffered an ACL tear as a result of a traumatic knee dislocation or patients who were conservatively managed were excluded from this study.
All patients underwent arthroscopic reconstruction of the ACL through a standard two portal arthroscopic procedure with ipsilateral semitendinosus and gracilis autograft. A longitudinal incision was used for the harvest. The harvested grafts were fixed in a four-strand, single bundle fashion with transverse cortico-cancellous femoral fixation with the Transfix® device and secured on the tibial side with a Bio-interference screw. The graft was fixed through a trans-tibial technique. All patients underwent standard post-reconstruction rehabilitation protocol and physician follow-up. Patients were put on an ACL brace post-operatively. Use of a brace was emphasized strictly for the first 6 weeks postoperatively. Patients started ambulation without the brace at 6 weeks and were gradually rehabilitated to treadmill running at approximately 12 weeks postoperatively. Patients were told not to return to sports earlier than 6 months postoperatively.
After Institutional Review Board approval was obtained, epidemiological data on the age, gender and body mass index (BMI) were obtained from the electronic health records of the patients. Specific variables extracted included the presence of concomitant MM and LM injuries intra-operatively, the patients’ level of intensity of sport (light, moderate, strenuous), duration of rehabilitation and mechanism of injury (contact, non-contact). Data regarding the patient’s level of intensity of sport was scored on a scale from 1 to 10 according to the activity rating survey that ranks sports and activities based on the risk of ACL injury and level of competition (17). Scores of 1–3 corresponded to “light” intensity of sports, 4–6 corresponded to “moderate” intensity of sport and a score of 7–10 corresponded to “strenuous” intensity of sport. For example, “strenuous” intensity indicated that the patient participated in sports at club, college, professional or elite levels involving jumping, twisting and pivoting motions such as basketball, rugby or football.
Results
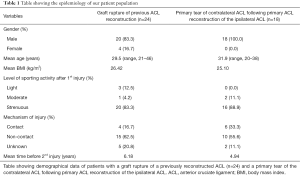
Of the 42 patients analyzed, 24 (57.1%) patients had graft rupture of a previously reconstructed ACL and 18 (42.9%) patients had a primary ACL tear of the contralateral knee following ACLR of the ipsilateral knee (Table 1).
Full table
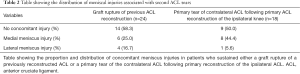
Of the 24 patients who suffered from a graft rupture of a previously reconstructed ACL, 20 (83.3%) were male, 4 (16.7%) were female, with a mean age of 29.5 years and mean BMI of 26.42 kg/m2. The mean time before re-injury was 6.18 years. Fifteen (62.5%) patients suffered a non-contact mechanism of injury whilst 4 (16.7%) patients suffered a contact injury. Twenty (83.3%) of patients had participated in a strenuous pre-injury level of sporting activity whilst 1 (4.2%) and 3 (12.5%) participated in moderate and light pre-injury levels of activity respectively. Ten (41.7%) patients had a concomitant injury of which, 6 (60.0%) were medial meniscal injuries and 4 (40.0%) were lateral meniscal injuries.
Of the 18 patients with a primary ACL tear on the contralateral knee, all patients were male, with a mean age of 31.9 years and mean BMI of 25.10 kg/m2. The mean time before re-injury was 4.94 years. Ten (55.6%) patients suffered a non-contact mechanism of injury whilst 6 (33.3%) patients suffered a contact injury. Sixteen (88.9%) of patients had participated in a strenuous pre-injury level of sporting activity whilst 2 (11.1%) participated in moderate pre-injury level of activity. Nine (50.0%) patients had a concomitant injury of which, 7 (77.8%) were medial meniscal injuries and 1 (11.1%) was a lateral meniscal injury. Data on concomitant injuries are detailed in Table 2.
Full table
Discussion
An ACL graft rupture or a primary ACL injury in the contralateral knee is one of the greatest concerns of patients following primary ACLR. The prospects of a repeated surgery and months of rehabilitation is daunting (10). Counseling patients on the risk of re-injuring either the reconstructed or the contralateral ACL along with the possibility of concomitant meniscal injuries is integral in the management of patients’ expectations during follow-up.
We hypothesized that a greater proportion of women would have suffered from a primary ACL injury of the contralateral knee as compared to graft rupture following ACLR of the ipsilateral knee. This hypothesis was backed by existing literature that consistently reported this trend (1,8,18). For example, Salmon et al. (19), in a cohort study of 100 men and 100 women found an overall incidence rate of injury to the ACL-reconstructed knee to be 8% for men and 4% for women and the rate of ACL injury to the contralateral knee to be 7% for women and 5% for men. Wright et al. (8) found that 86% of graft injuries of a previously reconstructed ACL occurred in males while 71% of injuries to the contralateral ACL following primary reconstruction of the ipsilateral ACL occurred in females. The etiology of the increased risk of ACL tears in the contralateral knee in women has been attributed to a smaller notch width, increased posterior tibial slope angle, and knee alignment with no concrete evidence (11-13,20).
In our present study, all (100%) patients who suffered a primary tear of the contralateral ACL following primary ACLR of the ipsilateral knee were male, which is in stark contrast to existing literature.
A variety of factors may contribute to the differences in ACL graft rupture and tears of the intact ACL in the contralateral knee rates noted between existing studies and this study. One consideration may be the age of the patients. The mean age of patients in the study performed by Wright et al. (8) was 24 years, while the mean age in our study was 29.5 years (range, 21–46 years) in patients who sustained a graft rupture and 31.9 years (range, 20–38 years) in patients who sustained a primary tear of the contralateral ACL follow primary reconstruction of the ipsilateral ACL. Beyond the age where women are enrolled in high school or college, the exposure rates to sports may be significantly reduced compared to men (18).
Of the 24 patients who sustained a graft rupture, we found that 41.7% (10/24) of patients also sustained a meniscal injury. This finding is similar, if not lower than reports in the literature on the rates of meniscal injuries in patients with an ACL tear for the first time. Maletius et al. (21), in an 18 to 24 year follow-up study of 60 patients found that 43% of patients had a concomitant meniscal injury. Kilcoyne et al. (22), in a retrospective study of 353 young athletes, found that 42% of patients with ACL injuries suffered at least one concomitant meniscal injury. Other studies have reported the rate of concomitant meniscal injuries to be as high as 82% in knees with acute ACL tears and as high as 96% in knees with chronic ACL tears (23,24). In addition, there was a higher rate of medial meniscus injuries (60%) as compared to lateral meniscus injuries (40%). This finding seems to reflect the distribution of meniscus injuries seen in chronically injured ACLs (24-28). This has been attributed to differences in translation patterns of the medial femoral condyle on the meniscal-tibial plateau in an ACL injured knee as compared to a healthy knee (23,29,30).
Of the 18 patients who suffered an ACL tear of the contralateral intact ACL, 50% (9/18) injured their meniscus as well. Likewise, this finding seems to be consistent with meniscal injury rates in patients who suffered a first ACL tear (21,22). The higher rate of medial meniscus injuries as compared to lateral meniscus injuries also seems to reflect the distribution of meniscus injuries seen in chronically injured ACLs (24-28).
This study is extremely relevant to reflect the demographics and location of 2nd ACL tears in the Asian population where the level of sporting activity in females may be much lower than in western populations. In addition, this study is the first to investigate and report the rate of ACL re-injury and concomitant meniscal injuries as a whole, instead of just isolated injuries. This is particularly useful when counseling a patient on the possibility of a meniscal injury and which meniscus is injured in the event that he/she presents with clinical or radiological findings suggestive of an ACL re-injury.
However, a limitation of this study was that patients who were conservatively managed were not included in this study. This is particularly important in delineating meniscal injury patterns, as it is well known that chronically injured ACL and acutely injured ACL present with different location and morphologies of meniscus injuries. Also, this study looked at re-injury rates on arthroscopy, which is more reflective of re-operation rates than the true re-injury rate, which might have been underestimated. There was also a lack of comparison of our results with existing literature in Asian populations. Additional studies that investigate the differences in knee anatomy of Asians and Caucasians and their impact on ACL injuries should be performed. In additional, studies that describe the rates of concomitant meniscal injuries in patients with a ruptured ACL graft or a rupture of a contralateral intact ACL should be performed for validation and comparison.
Conclusions
This study describes the demographics of 2nd ACL injuries in the Asian population. The female gender does not appear to be associated with a higher incidence of primary tears of the contralateral ACL in the Asian population. In addition, we also found that the rate of concomitant meniscal injuries in patients with a 2nd ACL tear is similar to the rate of concomitant meniscal injuries in a primary ACL rupture for the very first time.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Institutional Review Board.
References
- Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy 2005;21:948-57. [Crossref] [PubMed]
- Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med 2013;41:216-24. [Crossref] [PubMed]
- Ardern CL, Webster KE, Taylor NF, et al. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med 2011;39:538-43. [Crossref] [PubMed]
- Dunn WR, Spindler KP. MOON Consortium. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med 2010;38:2040-50. [Crossref] [PubMed]
- Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther 2010;40:141-54. [Crossref] [PubMed]
- Paterno MV, Rauh MJ, Schmitt LC, et al. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med 2012;22:116-21. [Crossref] [PubMed]
- Pinczewski LA, Lyman J, Salmon LJ, et al. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med 2007;35:564-74. [Crossref] [PubMed]
- Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med 2007;35:1131-4. [Crossref] [PubMed]
- Shelbourne KD, Benner RW, Gray T. Return to Sports and Subsequent Injury Rates After Revision Anterior Cruciate Ligament Reconstruction With Patellar Tendon Autograft. Am J Sports Med 2014;42:1395-400. [Crossref] [PubMed]
- Wright RW, Magnussen RA, Dunn WR, et al. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am 2011;93:1159-65. [Crossref] [PubMed]
- Harner CD, Paulos LE, Greenwald AE, et al. Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med 1994;22:37-43. [Crossref] [PubMed]
- Motohashi M. Profile of bilateral anterior cruciate ligament injuries: a retrospective follow-up study. J Orthop Surg (Hong Kong) 2004;12:210-5. [PubMed]
- Souryal TO, Moore HA, Evans JP. Bilaterality in anterior cruciate ligament injuries: associated intercondylar notch stenosis. Am J Sports Med 1988;16:449-54. [Crossref] [PubMed]
- Deehan DJ, Salmon LJ, Webb VJ, et al. Endoscopic reconstruction of the anterior cruciate ligament with an ipsilateral patellar tendon autograft. A prospective longitudinal five-year study. J Bone Joint Surg Br 2000;82:984-91. [Crossref] [PubMed]
- Roe J, Pinczewski LA, Russell VJ, et al. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 2005;33:1337-45. [Crossref] [PubMed]
- Sajovic M, Vengust V, Komadina R, et al. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med 2006;34:1933-40. [Crossref] [PubMed]
- Shelbourne KD, Jari S, Gray T. Outcome of untreated traumatic articular cartilage defects of the knee: a natural history study. J Bone Joint Surg Am 2003;85-A Suppl 2:8-16. [PubMed]
- Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med 2009;37:246-51. [Crossref] [PubMed]
- Salmon LJ, Refshauge KM, Russell VJ, et al. Gender differences in outcome after anterior cruciate ligament reconstruction with hamstring tendon autograft. Am J Sports Med 2006;34:621-9. [Crossref] [PubMed]
- Todd MS, Lalliss S, Garcia E, et al. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med 2010;38:63-7. [Crossref] [PubMed]
- Maletius W, Messner K. Eighteen- to twenty-four-year follow-up after complete rupture of the anterior cruciate ligament. Am J Sports Med 1999;27:711-7. [PubMed]
- Kilcoyne KG, Dickens JF, Haniuk E, et al. Epidemiology of meniscal injury associated with ACL tears in young athletes. Orthopedics 2012;35:208-12. [Crossref] [PubMed]
- Naranje S, Mittal R, Nag H, et al. Arthroscopic and magnetic resonance imaging evaluation of meniscus lesions in the chronic anterior cruciate ligament-deficient knee. Arthroscopy 2008;24:1045-51. [Crossref] [PubMed]
- Bellabarba C, Bush-Joseph CA, Bach BR Jr. Patterns of meniscal injury in the anterior cruciate-deficient knee: a review of the literature. Am J Orthop (Belle Mead NJ) 1997;26:18-23. [PubMed]
- Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am 1986;68:71-9. [PubMed]
- Warren RF, Levy IM. Meniscal lesions associated with anterior cruciate ligament injury. Clin Orthop Relat Res 1983.32-7. [PubMed]
- Thompson WO, Fu FH. The meniscus in the cruciate-deficient knee. Clin Sports Med 1993;12:771-96. [PubMed]
- Wickiewicz TL. Meniscal injuries in the cruciate-deficient knee. Clin Sports Med 1990;9:681-94. [PubMed]
- Glashow JL, Katz R, Schneider M, et al. Double-blind assessment of the value of magnetic resonance imaging in the diagnosis of anterior cruciate and meniscal lesions. J Bone Joint Surg Am 1989;71:113-9. [PubMed]
- von Eisenhart-Rothe R, Bringmann C, Siebert M, et al. Femoro-tibial and menisco-tibial translation patterns in patients with unilateral anterior cruciate ligament deficiency--a potential cause of secondary meniscal tears. J Orthop Res 2004;22:275-82. [Crossref] [PubMed]


