The importance of the regimen of screening in maximizing the benefit and minimizing the harms
Introduction
In CT screening for lung cancer, the regimen of screening is critical in diagnosing lung cancer early while limiting unnecessary tests and invasive procedures. This has been demonstrated by comparing two studies, one with a well-defined regimen of screening and the other which did not specify a regimen (1). The comparison of the two studies showed that the use of a regimen significantly increased the frequency of diagnosing stage I lung cancer and thus the resulting estimated cure rate and decreased the median tumor size of the cancers. Alternative explanations were postulated but these did not account for the differences in the results (1). The comparison also showed that the estimated cure rate resulting from annual CT screening is 80% or higher, a marked improvement over the rate of less than 10% when screening is not provided (1).
Critically important is that the regimen of screening remains state-of-the-art. Starting with the initial protocol developed for CT screening for lung cancer in 1992 (2-4), the protocol has been continuously updated based on the results of conferences held every 6 months (5,6) and on subsequent data emerging from CT screening (7-20). The protocol has been recently updated, integrating the latest technologies advances and knowledge (21).
Important in the development of the regimen is the recognition of the profound difference between the first, baseline round of screening and all subsequent rounds of repeat screening. For each person undergoing screening, the baseline round happens only once while repeat rounds will be performed annually for many years. This difference needs to be clearly recognized as it is these annual rounds which allow for identification of small, early, yet aggressive, lung cancers which have high cure rates despite their aggressiveness. In making the regimen, it has been well-demonstrated that tumor size and nodule consistency are key factors. In this chapter, we present our updated protocol (21) which is based on the cumulative results of the initial Lung Cancer Action Project (I-ELCAP) and its expanded successor program, the International Early Lung Cancer Action Program (I-ELCAP).
Identification of early stage lung cancers by CT screening also highlighted the need to updating of the pathologic criteria for lung cancer. For this reason, the I-ELCAP investigators held multiple pathology conferences at which the screen-detected lung cancers were reviewed (22-25). These reviews in turn led to the formation of a multi-disciplinary team led by Travis which has developed new terminology and updated pathologic criteria (26-28).
Innovations in treatment of early stage lung cancer are also a consequence of CT screening. Video-assisted thoracic surgery (VATS) is rapidly replacing thoracotomy for early stage lung cancer (29). Increasingly, limited resection and limited mediastinal lymph node dissection is being performed for certain subtypes of lung cancer (29-32).
A summary of the process from the initial studies of CT screening to its national implementation for high-risk smokers which has been a long process of over 25 years is given in another publication (33). The hope is that the experience will be beneficial in speeding up the introduction of new screening, biomarker, and diagnostic tests as well as therapeutic approaches in the future.
Lead-time, length and overdiagnosis bias
Possible biases that affect the cure rate estimates obtained from the ELCAP design are: lead-time, length and overdiagnosis (33). Lead-time is defined as the time by which the diagnosis under screening is advanced when compared to when it is made in the absence of screening. If the screening test provides for no lead-time, it provides no advantage. Lead-time bias exists when the cure rate is estimated using a KM survival rate before the curve reaches its asymptotic value. However, once the asymptotic value is reached, the Kaplan-Meier estimates of cure rate no longer have lead-time bias (9).
Overdiagnosis, according to the usual definition, occurs when screening leads to diagnosis of a lung cancer and that cancer, if not diagnosed or treated, would not have led to death. This can occur in two ways: (I) diagnosing a cancer, that even though it is a genuine life-threatening cancer, does not cause death because (s)he dies of a competing causes (e.g., automobile accident, myocardial infarction) (11), these can be slow-growing or (II) diagnosing a lung cancer that is genuinely indolent and it does not lead to death in the absence of treatment. Dying of competing causes of death (the first point) is partially addressed by choosing the appropriate indications for screening (e.g., age, fit to undergo thoracic surgery, at least a 5 or 10-year life expectancy) (11). The ELCAP design focuses on the second point in several ways by: (I) requiring documentation of growth, at a malignant rate, for nodules less than 15 mm in size prior to recommendation for further invasive testing (www.IELCAP.org); (II) assessing the growth rates of the lung cancers diagnosed under the screening (34-38); and (III) having an expert pathology panel review of the resected pathologic specimens (22-25) to confirm that the resected specimens represented genuine lung cancers.
We also followed participants who have documented cancer but chose not to be treated to determine their outcome. If a certain category of diagnosed lung cancers are considered to be sufficiently slow-growing based on any of the above approaches, they can be excluded from the KM survival analysis of the genuine, aggressive lung cancers. For example, typical carcinoids, as they are slow growing and are not always resected, have been excluded from the published survival analysis in I-ELCAP (9). If, however, there is still concern regarding inclusion of overdiagnosed cases then further exclusions can be made. For example, by excluding all diagnosis of adenocarcinoma having 90% or more bronchioloalveolar features, the overall cure rate in I-ELCAP was reduced from 80% to 78%.
A third bias, “length bias”, exists in all screening programs for cancer. It exists as a single round of screening, the baseline round, will identify a higher proportion of slow-growing cancers than faster-growing ones. Thus the distribution of cancer subtypes resulting from the baseline round of screening is different than the distribution of cancers in the absence of screening. On the other hand, the distribution of cancer subtypes on the subsequent repeat rounds of screening should reflect the distribution in the absence of screening. Length bias is addressed by analyzing the baseline and repeat rounds of screening separately (9,12). Such an analysis will show that distribution by cancer cell-types is different in the baseline round than in repeat rounds and these differences provide valuable information on the relative aggressiveness of the different cell-types. For example, the proportion of small-cell and squamous-cell increases in annual rounds than in the baseline round, consistent with these cell-types being more aggressive (9,12).
Regimen of screening
Detailed below are the key specifications of the current I-ELCAP regimen of screening (21). The actual regimen is summarized in Figures 1 and 2. Detailed information as to image production, reading, and assessment is given below.
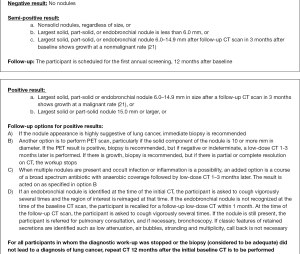

Image production
The low-dose CT imaging is the same in baseline and repeat screenings. As there are a large variety of CT manufacturers and models which have markedly improved resolution and other capabilities over time, the following are general guidelines for the image production. Scans should be acquired on m16-detector-row scanners. Scans should be acquired so that images can be reconstructed at 1.25 mm or less.
There is no specific definition of “low-dose”. Historically most screening protocols have used scan parameters of 120–140 kVp and 30–100 mAs, but it is suggested that the scans are obtained at 120 kVp or lower and 40 mAs (effective) or lower. Scan parameters should also be adjusted to allow for different size patients. Dose modulation techniques which adjust for body size are available on most modern scanners. These should be established based either on weight or body mass index. In addition, new dose reduction techniques are being made available by scan manufacturers, and their use is encouraged, providing that acceptable image quality is maintained. Guidance on scan parameters specific to manufacturers make and model can be found on the website of the American Association of Physicists in Medicine (http://www.aapm.org/pubs/CTProtocols/?tab=5#CTabbedPanels).
Images should be acquired in a single breath from the lung apices through the lung bases. Standards should be established to ensure consistent breath holding. Contrast material is not used. Just prior to acquiring the low-dose CT scan, the participant should be asked to cough vigorously several times to clear the trachea and major bronchi of possible mucus secretions and avoid additional imaging that might be required to distinguish such secretions from endobronchial lesions.
Follow-up imaging of abnormalities identified as a result of screening should typically be performed using the same low dose parameters used for the baseline and repeat screenings.
Reading of images
The images are read by a radiologist who is aware of the round of screening (baseline or repeat) from which the images derive. The reader views the images as they are displayed in a high-resolution monitor at their typical window and level settings, scrolling through the images one at a time. For the purposes of assessing the size of a nodule or that of a mediastinal abnormality, however, the following settings are used: lung window width 1,500 HU and lung window level −650 HU, and mediastinal window width 350 HU and mediastinal window level 25 HU.
In both baseline and repeat screening, the reader’s first concern is to identify all non-calcified nodules (NCNs) visible in the images. In addition, on repeat screenings, the reader’s special concerns are to identify all new NCNs and those that produced a semi-positive result on the initial CT at baseline and show growth since then, either in the overall size of a solid nodule or in the solid component of a part-solid nodule, or in the development of a solid component within a previously nonsolid nodule. To determine whether growth has occurred, the reader compares the current images with the corresponding previous ones, displayed side-by-side.
For each of these nodules in the lung parenchyma or bronchi, the location, size, consistency (‘solid’, ‘part-solid’ or ‘nonsolid’), calcifications, nodule edge characteristics, including spiculations are specified.
Definition of nodule and noncalcified nodules
A nodule is a focal non-linear opacity with a generally spherical shape surrounded by lung parenchyma. It is classified as non-calcified if it fails to meet the usual criteria for benign, calcified nodules (21).
Definition of nodule consistency
A nodule is classified solid unless it has specific characteristics to be classified as subsolid (21). Solid nodules may have external or internal cystic airspace or internal cavitation (15). Subsolid nodules may be either nonsolid or part-solid (7,19,20). A part-solid nodule is one that has internal components that completely obscure the lung parenchyma, and non-solid if none of the lung parenchyma is completely obscured. In making the distinction between part-solid and nonsolid nodule, blood vessels within the nodule, despite their appearance as solid components, are not regarded as solid components. Part-solid nodules are nodules which typically start as nonsolid nodules and subsequently develop an internal solid component. The workup of subsolid nodules should be based on the size of the largest solid component (19,20,26-28). This recommendation is based on the radiologic findings as well as the pathology findings.
The distinction between part-solid and solid may be difficult, particularly when the progression from nonsolid to part-solid cannot be confirmed as prior images are not available. Thus, when the diameter of the solid component relative to the diameter of the entire nodule is 80% or more and the progression cannot be verified, the nodule should be classified as solid (20).
Definition of nodule size
Nodule size is reported according to the nodule diameter. The nodule diameter is the average of its length and width. Length is measured on a single CT image (axial, sagittal, or coronal) that shows the maximum length; width, defined as the longest perpendicular to the length, is measured on the same CT image. The diameter of the solid component of part-solid nodules is also documented in the same way.
These diameter measures should be supplemented by computer-based assessments of volume, although such automated measures need to be interpreted cautiously as these are still considered experimental (34-38). When there is sufficient evidence of their validity and accuracy, volume measures should replace manual diameter measurements.
Probability of lung cancer by nodule size and consistency
The nodule size thresholds for definition of positive result are continually reevaluated and have changed since the start of ELCAP. Initially there was no size cutoff for positive results (3,4), thresholds have been introduced since then and updated multiple times because of advancing technology and accumulating evidence (8,18). In the current protocol, the nodule diameter threshold for positive result is 6 mm on baseline and 3 mm on annual repeat screening, but future updates are anticipated.
It has been shown that some solid and many subsolid nodules identified in the lung parenchyma will resolve, particularly new ones identified on repeat screenings (19,20). Thus, follow-up imaging three [3] months after baseline or one [1] month after annual repeat screening is useful to avoid unnecessary further diagnostics, especially invasive ones.
The frequency of malignancy by nodule size is different in the baseline round than in annual repeat rounds. For smaller size nodules, the probability of malignancy is higher on annual repeat screening than on baseline screening. Also the probability of malignancy is lower for the larger size nodules on annual repeat screening. The frequency with which such nodules are cancers is not known, especially among those nonsolid nodules, as diagnosis has not have been pursued in all cases. However, based on review over the I-ELCAP experience past 20 years, there was no diagnosis of malignancy on annual repeat rounds in new nonsolid nodules greater than 15 mm or in part-solid nodules greater than 31+ mm (19,20).
Assessment of growth
Growth of a nodule is defined as: (I) enlargement of the overall nodule size regardless of consistency; (II) growth of the solid component of a part-solid nodule; (III) development of a solid component within a nonsolid nodule; and (IV) increased attenuation of nonsolid components of a nonsolid nodule. Growth is assessment by measuring the maximum length and the perpendicular width of the nodule using the CT image of the nodule. The diameter is calculated as the average of the measured length and width and this is again done on the follow-up images. These two diameter measurements at two time points is used to calculate the volume doubling time (VDT) of the nodule (14,34-38). VDTs of less than 30 days are more suggestive of an infection than malignancy. Lung cancer VDTs are more than 30 days, typically between 30 and 400 days. VDTs also provide an excellent alternative to PET scans for assessment of malignancy and where used extensively prior to the availability of PET scans. VDTs have been successfully introduced used in the screening regimen of the NELSON, a randomized trial of CT screening being performed in the Netherlands (39).
The use of VDTs requires understanding of the inherent measurement error of the CT measurements. VDTs are based on the change in the nodule length, width, and height, but it must be recognized that accurate determination of these measurements on CT are influenced by multiple factors including not only the intrinsic properties of the nodule itself, but also of the CT scanner and its adjustable scanner parameters, and the software used to make the measurement and these factors interact in complex ways (40). Several groups have developed approaches to incorporate measurement errors into the determination of growth. The RSNA’s Quantitative Imaging Biomarkers Alliance (QIBA) is in the final stages of releasing their recommendations (41) and has made a web-based calculator available at http://accumetra.com/solutions/qiba-lung-nodule-calculator. The American College of Radiology (ACR) specifies growth for a nodule of any size requires “an increase of 1.5 mm or more” (42,43). Both the QIBA and ACR approaches allow for large degrees of measurement error to cover a wide range of CT scanners and the protocols. I-ELCAP protocol also provides guidance as to assessment of growth (21).
Computer assisted evaluation of growth rates and volume doubling times is still a topic of research. The computer scans and the segmentation should be inspected for image quality (e.g., motion artifacts) and for the quality of the segmentation. The radiologist should visually inspect both nodule image sets side-by-side to verify the quality of the computer segmentation for each image that contains a portion of the nodule. The segmentations should also be examined for errors such as when a vessel is segmented as part of a nodule in one scan but not in the other. Scan slice thickness for the purpose of volumetric analysis should not exceed 1.25 mm.
While these estimates are meant only as boundaries to be confident that actual change has occurred, they do not provide accuracy as to a particular rate of growth. At this point, decisions regarding confidence intervals about determining malignant growth rates within specified time intervals remains a topic of research.
Documentation and quality control
The background information, findings on each of the CT scans and follow-up recommendations are documented in a web-based system which is accessible by internet throughout the world (44).
Other findings on the CT scan
Smoking cessation information and advice should be provided in all screening programs. The screening presents “a teachable moment” each year and it has been shown that over time, smoking decreases (45-47).
Other findings on the CT scan of the chest should also be reported and these include the presence of discrete cystic airspaces because when the walls of these airspaces show progressive thickening, both in increasing thickness and increasing circumferential wall involvement, these maybe due to lung cancer (15).
The extent of emphysema is identified and classified as none, mild, moderate, or severe, each being scored 0 to 3, respectively. Mild emphysema is defined by having no discrete areas of decreased CT attenuation but splaying of blood vessels suggesting parenchymal expansion or having occasional discrete areas of decreased attenuation; moderate emphysema if discrete areas of decreased attenuation can be identified involving less than half of the lung parenchyma; and, severe emphysema if discrete areas of decreased attenuation can be identified involving more than half of the lung parenchyma. Each subject receives an emphysema score in the range from 0 to 3 (48). If emphysema is present and previously unrecognized, consultation with a pulmonologist is recommended (48).
Early findings of usual interstitial pneumonitis (UIP) have been classified as pre-honeycomb and honeycomb (HC) findings (49). Other interstitial diseases can also be identified and may differ in location and findings (50). Pre-honeycomb findings may start with traction bronchiectasis alone and then progress to ground-glass opacification and reticulations, typically at the periphery of the lungs and at the lung bases. The likelihood of disease progression is associated with honeycombing and early identification is important so when such findings are present, consultation with a pulmonologist is recommended.
Mediastinal masses can occur anywhere in the mediastinum, including in the thymus, heart, and esophagus; and masses in the neck, such as the thyroid, may extend into the mediastinum. Such mediastinal and soft tissues masses are documented as to location and size. Based on the frequency and natural course of thymic masses identified in baseline and annual repeat screenings for lung cancer (51), the following work-up recommendations are made: if the mass is less than 3.0 cm in diameter on baseline CT without invasive features (e.g., irregular borders or loss of fat planes), follow-up CT one year later is recommended. If the thymic mass is greater than 3.0 cm or shows growth on the follow-up CT, then further workup according to standard practice is recommended.
Each coronary artery should be identified (main, left anterior descending, circumflex, and right). Evidence of calcification in each artery is documented as none, minimal, moderate, or severe, scored as 0, 1, 2, and 3, respectively. Minimal calcification was defined if less than 1/3 of the length of the entire artery, moderate as 1/3–2/3, and severe as more than 2/3 shows calcification. With 4 arteries thus scored, each subject received an Ordinal CAC Score in the range from 0 to 12 and the corresponding recommendations are given in the section on the workup of ancillary findings (52-56). Currently, it is also possible to obtain the Agatston, volume or mass calcium scores on low-dose CT scans and then the standard Agatston recommendations can be used. New rapid scanning techniques minimize cardiac motion and allow for improved Agatston scoring on non-gated examinations. However, the equivalence of these Ordinal scores, based on analyses of screening data showed there is excellent agreement in the ordinal CAC score for the categories of the Agatston scores (54).
CT images also show the breast tissue and can be classified according to the Breast Imaging Reporting and Data System (BI-RADS) developed by the American College of Radiology (Sickles EQ, D’Orsi CJ, Basett LW, et al. ACR 2013, 4th edition). The BI-RADS classification identifies 4 grades according to the breast density. Grade 1: breasts are almost entirely fatty; grade 2: breasts are composed of scattered fibroglandular densities; grade 3: breasts are heterogeneously dense, which may obscure small masses, and grade 4: breasts are extremely dense, which lowers the sensitivity of mammography. The key differentiation is between grades 1–2 and 3–4 (57). If the percentage of breast tissue is, grade 3 or grade 4, then this should be noted in the report as it suggests an increased risk for breast cancer and if clinically indicated, ultrasound or MRI of the breast is suggested as the mammogram might obscure an early cancer or precursor lesion.
Classification and characterization of diagnosed cancers
A diagnosis (rule-in) of lung cancer is classified as a baseline screen-diagnosed lung cancer if the nodule is identified on the initial CT on baseline, regardless of when the diagnosis actually is achieved (9,21). It is classified in this way also if the result was ‘semi-positive’ and thus an annual repeat CT 12 months later was recommended. If the result of the initial CT at baseline is negative and diagnostic work-up is prompted by suspicion-raising symptoms (or an incidental finding) before the scheduled first annual repeat screening, the diagnosed cancer is classified as a baseline interim-diagnosis, again regardless of when the diagnosis is achieved.
Analogous attributions are applied in the context of repeat-screening cycles. If lung cancer is diagnosed in a new nodule that was first identified on annual repeat, it is an annual repeat screen-diagnosed cancer, even if it is seen on the baseline screening in retrospect but was not identified at that time (9,21). If work-up is prompted by suspicion-raising symptoms (or an incidental finding) in between annual screening, the diagnosed cancer is classified as an annual interim-diagnosis.
Each diagnosed cancer is characterized according to indicators of how early and otherwise significant the cancer is—all of this bearing on the prognostic issues (21). Principal among these descriptors/indicators is the clinical stage of the disease at diagnosis. Clinical stage I, for purposes of further research is defined by the size of the tumor (T status), no manifestations of lymph node metastases in the hila, mediastinum (N status), and supraclavicular or axillary regions, or distant metastases in adrenals, liver, spleen, bones, or soft tissues visible in the chest CT and no signs of metastases on PET scan, if performed (M status). The presence/absence of lymph-node and distant metastases (N and M status) is assessed on the most recent CT scan prior to treatment, and also from a PET scan, if available. The person is classified as being of clinical stage I as long as these imaging studies do not demonstrate evidence of lymph node or distant metastases (N0M0), or other invasive non-adenocarcinomas, even when there is more than 1 adenocarcinoma, all less than 30 mm in diameter (9,21,25).
Conclusions
The I-ELCAP collaboration provides a new paradigm that answers the 2002 NCI call for multiple approaches to address all relevant questions about screening (58) and the Institute of Medicine (IOM) Roundtable on Evidence-based Medicine from the National Academy of Science’s call (59) for a “new clinical research paradigm that takes better advantage of data generated in the course of healthcare delivery would speed and improve the development of evidence for real-world decision making”.
In response to the results provided by ELCAP in 1999 (3), the National Cancer Institute decided to perform a randomized trial, the National Lung Screening Trial (NLST) to provide further evidence about CT screening for lung cancer (60-62). Randomized trials for evaluation of alternative treatments had been introduced in the late 1950’s and had been useful in rigorous evaluation of treatment alternatives. The approach had been expanded to be used for evaluation of screening tests, particularly for breast, lung, and prostate cancer (63,64). These types of trial, however, proved to be more complicated and often resulted in further controversies (65-74). Learning from previous screening trials, the NLST design called for 50,000 participants who were randomly assigned to 3 years of screening with CT scans or chest radiographs. The NLST was launched in 2002 and ended in 2008. CT screening was powerful enough to show a mortality reduction despite the limited number of rounds of screening and it also was the first randomized trial to show an all-cause mortality reduction, but it took another 3 years before the results were published (62). Despite the concerns about the study design, the NLST was highly successful in demonstrating the benefit of CT screening. In response to the compelling NLST results and those of prior studies from ELCAP and Japan as well as other smaller studies in Europe, the United States Preventive Services Task Force decided to recommend CT screening for high risk smokers (75).
I-ELCAP has continued to provide screening and thus has been able to continually introduce updates in the regimen of screening. It has enrolled more than 70,000 participants worldwide, aged 40 years and older who are current, former, or never smokers with occupational or environmental exposure to known carcinogens.
The I-ELCAP collaboration stimulated development of entirely new research domains as already mentioned, including computer assisted 3D nodule growth analysis, smoking cessation in the context of screening, measuring extent of emphysema, quantifying coronary calcium on low-dose scans as a measure of cardiac disease, quantifying breast density on low-dose CT, and evaluating early interstitial lung disease.
The ELCAP study design presents a challenge to the traditional view of the supremacy of the randomized trial in the evaluation of the effectiveness of screening. Even in 2002, when the National Cancer Institute launched the NLST, the NCI understood that no single approach would answer all relevant questions and recommended that multiple approaches be pursued (58). The IOM report (59) also recognized the limitations of the randomized trial, stating that “as useful as it is under the right circumstances, (it) takes too much time, is too expensive, and is fraught with questions of generalizability”. The IOM report also addressed the need to better characterize the range of alternatives to the randomized trial (e.g., quasi-experimental trials), and their applications and implications.
We suggest that the ELCAP design and its protocol which allows for pooling of data on a global basis and allows for quasi-experimental assessment of treatments is such a new paradigm. It was designed to provide data in screening for a cancer in a clinical setting that can be readily translated into a widespread screening program. It provided a protocol that generated data in the course of healthcare delivery to be collected, pooled, and analyzed so that the regimen of screening could be continually updated.
Randomized trials, when properly designed and implemented, provide important evidence for testing the hypothesis of a mortality reduction from preventive and screening efforts, but as stated by the IOM (59), they are very costly and require much time as evidenced by the National Lung Screening Trial (NLST) (62). Also randomized screening trial use cumulative mortality reduction as their outcome parameter and this actual value of this parameter depends on the number of rounds of screening that are provided and on how it is assessed. This outcome parameter provides an underestimate of the case fatality of the cancer under screening, that is, it is a bias estimate of the actual benefit of the screening being evaluated (69,70,72-74). Thus, randomized trials have a propensity to lead to incorrect negative trial results unless carefully designed and executed, and even when positive (i.e., the null hypothesis is rejected) results is an underestimate of the true mortality reduction provided by the screening. In addition, factors affecting the estimates, such as protocol non-adherence, must also be addressed. Also, randomized trials cannot address the full spectrum of effects of a complex diagnostic process followed by treatment which aims to modify the natural history of a disease. Even in the best designed randomized trial, ethical considerations require the investigators to modify the control arm. For example, instead of control arm of the NLST being the current standard of not providing any screening, chest X-ray screening was used and it probably does have some benefit thus decreasing the observed difference between the mortality rates of the two arms (62). The impact of these design factors need to be clearly stated and estimates of their influence should be provided when presenting results of these trials.
The NLST was initiated due to the compelling evidence demonstrated in the ELCAP report in 1999 (3). It rekindled interest in screening for lung cancer. Due to the strength of the results, the NLST was rapidly funded and started in 2002. During the 8 years of conducting the trial, the NLST has cost over 300 million dollars to provide a qualitatively correct answer which together with other studies led to the recommendations by the United States Preventive Services Task Force to provide CT screening for high risk smokers (75). Unfortunately, the mortality reduction of 20% has been misinterpreted as to its meaning. Mortality rates as estimated from randomized trials do not provide cure rates and thus there is no inherent incompatibility between a 20% mortality reduction from a randomized trials with 3 rounds of screening and an average of 5 years of follow-up provided by the NLST (62), and the 80% estimated cure rate provided by the ELCAP design (3,9). Mortality rates provided by randomized screening trials will always underestimate the cure rate of the screening (69-74) but this fails to be recognized in the statements of the benefit of the screening (76). In the absence of screening, the fatality rate (1-cure rate) of 90% from lung cancer has continued. Public funds for non-randomized screening studies were nearly impossible to obtain because of the commitment to the dominant paradigm of the randomized trial. We believe that the I-ELCAP and NLST “story” provides a strong argument for relevant agencies to reconsider the priorities for the public funding of studies aimed at evaluating the effectiveness of screening and other medical trials. To achieve this end, a dialogue should be encouraged between the investigators involved in the different types of studies in order to secure the maximum benefit from all approaches, and thereby create a balanced funding portfolio for different designs in support of research on cancer screening.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Yankelevitz is a named inventor on a number of patents and patent applications relating to the evaluation of diseases of the chest including measurement of nodules. Some of these, which are owned by Cornell Research Foundation (CRF), are non-exclusively licensed to General Electric. As an inventor of these patents, Dr. Yankelevitz is entitled to a share of any compensation which CRF may receive from its commercialization of these patents. He also serves on the scientific advisory board (unpaid) for Give-A-Scan, Lung Cancer Alliance and serves as a consultant for Accumetra, LLC; Dr. Henschke is the President and serves on the board of the Early Diagnosis and Treatment Research Foundation. She receives no compensation from the Foundation. The Foundation is established to provide grants for projects, conferences, and public databases for research on early diagnosis and treatment of diseases. Dr. Claudia Henschke is also a named inventor on a number of patents and patent applications relating to the evaluation of pulmonary nodules on CT scans of the chest which are owned by Cornell Research Foundation (CRF). Since 2009, Dr. Henschke does not accept any financial benefit from these patents including royalties and any other proceeds related to the patents or patent applications owned by CRF; Dr. Salvatore works for the Speakers Bureau for Genentech, specifically for interstitial lung disease; other authors have no conflicts of interest to declare.
References
- Yip R, Henschke CI, Yankelevitz DF, et al. The impact of the regimen of screening on lung cancer cure: a comparison of I-ELCAP and NLST. Eur J Cancer Prev 2015;24:201-8. [Crossref] [PubMed]
- Henschke CI, Miettinen OS, Yankelevitz DF, et al. Radiographic screening for cancer: Proposed paradigm for requisite research. Clin Imaging 1994;18:16-20. [Crossref] [PubMed]
- Henschke CI, McCauley DI, Yankelevitz DF, et al. Early Lung Cancer Action Project: overall design and findings from baseline screening. Lancet 1999;354:99-105. [Crossref] [PubMed]
- Henschke CI, Naidich DP, Yankelevitz DF, et al. Early Lung Cancer Action Project: preliminary findings on annual repeat screening. Cancer 2001;92:153-9. [Crossref] [PubMed]
- International Early Lung Cancer Action Program Conferences and Consensus Statements. Available online: http://events.ielcap.org/conferences/past. Accessed March 15, 2016.
- Henschke CI, Yankelevitz DF, Smith JP, et al. Screening for lung cancer: the Early Lung Cancer Action approach. Lung Cancer 2002;35:143-8. [Crossref] [PubMed]
- Henschke CI, Yankelevitz DF, Mirtcheva R, et al. CT screening for lung cancer: Frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 2002;178:1053-7. [Crossref] [PubMed]
- Henschke CI, Yankelevitz DF, Naidich DP, et al. CT screening for lung cancer: Suspiciousness of nodules according to size on baseline scans. Radiology 2004;231:164-8. [Crossref] [PubMed]
- International Early Lung Cancer Action Program Investigators, Henschke CI, Yankelevitz DF, et al. Survival of Patients with Stage I lung cancer detected on CT screening. N Engl J Med 2006;355:1763-71. [Crossref] [PubMed]
- Henschke CI, Shaham D, Yankelevitz DF, et al. CT Screening for Lung Cancer: Significance of diagnoses in the baseline cycle of screening. Clin Imaging 2006;30:11-5. [Crossref] [PubMed]
- Henschke CI, Yip R, Yankelevitz DF, et al. CT screening for lung cancer: competing causes of death. Clin Lung Cancer 2006;7:323-5. [Crossref] [PubMed]
- Henschke CI, Yankelevitz DF, Miettinen OS, et al. Computed tomographic screening for lung cancer: the relationship of disease stage to tumor size. Arch Intern Med 2006;166:321-5. [Crossref] [PubMed]
- New York Early Lung Cancer Action Project Investigators. CT Screening for lung cancer: diagnoses resulting from the New York Early Lung Cancer Action Project. Radiology 2007;243:239-49. [Crossref] [PubMed]
- Henschke CI, Yankelevitz DF, Yip R, et al. Lung Cancers Diagnosed at Annual CT Screening: Volume Doubling Times. Radiology 2012;263:578-83. [Crossref] [PubMed]
- Farooqi AO, Cham M, Zhang L, et al. Lung cancer associated with cystic airspaces. AJR Am J Roentgenol 2012;199:781-6. [Crossref] [PubMed]
- Austin JH, Yip R, D'Souza BM, et al. Small-cell carcinoma of the lung detected by CT screening: stage distribution and curability. Lung Cancer 2012;76:339-43. [Crossref] [PubMed]
- Xu DM, Yip R, Smith JP, et al. Retrospective review of lung cancers diagnosed in annual rounds of CT screening. AJR Am J Roentgenol 2014;203:965-72. [Crossref] [PubMed]
- Henschke CI, Yip R, Yankelevitz DF, et al. Definition of a positive test result in computed tomography screening for lung cancer: a cohort study. Ann Intern Med 2013;158:246-52. [Crossref] [PubMed]
- Yankelevitz DF, Yip R, Smith JP, et al. CT Screening for Lung Cancer: Nonsolid Nodules in Baseline and Annual Repeat Rounds. Radiology 2015;277:555-64. [Crossref] [PubMed]
- Henschke CI, Yip R, Wolf A, et al. CT Screening for Lung Cancer: Part-solid Nodules in Baseline and Annual Repeat Rounds. Insights Imaging 2015;6:S278.
- International Early Lung Cancer Action Program protocol. Available online: http://www.ielcap.org/sites/default/files/I-ELCAP%20protocol-v21-3-1-14.pdf. Accessed March 23, 2016.
- Vazquez M, Flieder D, Travis W, et al. Early Lung Cancer Action Project pathology protocol. Lung Cancer 2003;39:231-2. [Crossref] [PubMed]
- Flieder DB, Vazquez M, Carter D, et al. Pathologic findings of lung tumors diagnosed on baseline CT screening. Am J Surg Pathol 2006;30:606-13. [Crossref] [PubMed]
- Carter D, Vazquez M, Flieder DB, et al. Comparison of pathologic findings of baseline and annual repeat cancers diagnosed on CT screening. Lung Cancer 2007;56:193-9. [Crossref] [PubMed]
- Vazquez M, Carter D, Brambilla E, et al. Solitary and Multiple Resected Adenocarcinomas after CT Screening for Lung Cancer: Histopathologic Features and their Prognostic Implications. Lung Cancer 2009;64:148-54. [Crossref] [PubMed]
- Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung cancer/American Thoracic Society/European Respiratory Society International Multidisciplinary Classification of Lung Adenocarcinoma. J Thorac Oncol 2011;6:244-85. [Crossref] [PubMed]
- Travis WD, Brambilla E, Burke AP, et al, editors. WHO classification of tumours of the lung, pleura, thymus and heart. Lyon: International Agency for Research on Cancer, 2015.
- Travis WD, Asamura H, Bankier A, et al. The IASLC lung cancer staging project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol 2015. [Epub ahead of print].
- Flores R, Bauer T, Aye R, et al. Balancing curability and unnecessary surgery in the context of CT screening for lung cancer. J Thorac Cardiovasc Surg 2014;147:1619-26. [Crossref] [PubMed]
- Altorki NK, Yip R, Hanaoka T, et al. Sub-lobar resection is equivalent to lobectomy for clinical Stage IA lung cancer in solid nodules. J Thorac Cardiovasc Surg 2014;147:754-62; discussion 762-4. [Crossref] [PubMed]
- Buckstein M, Yip R, Yankelevitz D, et al. Radiation therapy for Stage I lung cancer detected on computed tomography screening: results from the International Lung Cancer Action Program. J Radiat Oncol 2014;251:1-5.
- Flores RM, Nicastri D, Bauer T, et al. CT Screening for Lung Cancer: Mediastinal lymph node resection in Stage IA non-small cell lung cancer manifesting as subsolid and solid nodules. Ann Surg 2016. In Press.
- Henschke CI, Boffetta P, Yankelevitz DF, et al. CT screening: the International Early Lung Cancer Program Experience. Thorac Surg Clin 2015;25:129-43. [Crossref] [PubMed]
- Kostis WJ, Yankelevitz DF, Reeves AP, et al. Small pulmonary nodules: reproducibility of three-dimensional volumetric measurement and estimation of time to follow-up CT. Radiology 2004;231:446-52. [Crossref] [PubMed]
- Yankelevitz DF, Kostis WF, Henschke CI, et al. Overdiagnosis in chest radiographic screening for lung carcinoma: Frequency. Cancer 2003;97:1271-5. [Crossref] [PubMed]
- Yankelevitz DF, Gupta R, Zhao B, et al. Repeat CT Scanning for Evaluation of Small Pulmonary Nodules: Preliminary Results. Radiology 1999;212:561-6. [Crossref] [PubMed]
- Yankelevitz DF, Reeves A, Kostis W, et al. Determination of malignancy in small pulmonary nodules based on volumetrically determined growth rates: Preliminary results. Radiology 2000;217:251-6. [Crossref] [PubMed]
- Reeves AP, Chan A, Yankelevitz D, et al. On measuring the change in size of pulmonary nodules. IEEE Trans Med Imaging 2006;25:435-50. [Crossref] [PubMed]
- van Klaveren RJ, Oudkerk M, Prokop M, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med 2009;361:2221-9. [Crossref] [PubMed]
- Avila R, Yankelevitz D, Archer V, et al. Calibration of computed tomography (CT) volumetric measurements for assessing tumour response to drug therapy in a randomized multicentre oncology study. Insights Imaging 2013;4:S331.
- Armato SG 3rd, McLennan G, McNitt-Gray MF, et al. Lung image database consortium: developing a resource for the medical imaging research community. Radiology 2004;232:739-48. [Crossref] [PubMed]
- Kazerooni EA, Austin JH, Black WC, et al. ACR-STR practice parameter for the performance and reporting of lung cancer screening thoracic computed tomography (CT): 2014 (Resolution 4). J Thorac Imaging 2014;29:310-6. [Crossref] [PubMed]
- Kazerooni EA, Armstrong MR, Amorosa JK, et al. ACR CT accreditation program and the lung cancer screening program designation. J Am Coll Radiol 2015;12:38-42. [Crossref] [PubMed]
- Reeves AP, Kostis WJ, Yankelevitz DF, et al. A web-based database system for multi-institutional research studies on lung cancer. Radiologic Society of North America Scientific Session. Chicago, IL. November 27, 2001.
- Ostroff JS, Buckshee N, Mancuso CA, et al. Smoking Cessation: An unexpected benefit of Screening CT for Detection of Early Lung Cancer. Prev Med 2001;33:613-21. [Crossref] [PubMed]
- Anderson CM, Yip R, Henschke CI, et al. Smoking cessation and relapse during a lung cancer screening program. Cancer Epidemiol Biomarkers Prev 2009;18:3476-83. [Crossref] [PubMed]
- Ostroff JS, Henschke CI, Yip R, et al. Smoking cessation among current smokers following enrollment in a lung cancer screening program. Cancer Epidemiol Biomarkers Prev 2015. In Press.
- Zulueta JJ, Wisnivesky JP, Henschke CI, et al. Scoring of Emphysema detected on low-dose CT Predicts Death from Chronic Obstructive Pulmonary Disease and Lung Cancer. Chest 2012;141:1216-23. [Crossref] [PubMed]
- Salvatore M, Henschke CI, Yip R, et al. JOURNAL CLUB: Evidence of Interstitial Lung Disease on Low-Dose Chest CT Images: Prevalence, Patterns, and Progression. AJR Am J Roentgenol 2016;206:487-94. [Crossref] [PubMed]
- Southern BD, Scheraga RG, Yadav R. Managing interstitial lung disease detected on CT during lung cancer screening. Cleve Clin J Med 2016;83:55-65. [PubMed]
- Henschke CI, Lee IJ, Wu N, et al. CT screening for lung cancer: prevalence and incidence of mediastinal masses. Radiology 2006;239:586-90. [Crossref] [PubMed]
- Shemesh J, Henschke CI, Farooqi A, et al. Frequency of coronary artery calcification on low-dose computed tomography screening for lung cancer. Clin Imaging 2006;30:181-5. [Crossref] [PubMed]
- Shemesh J, Henschke CI, Shaham D, et al. Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest predicts deaths from cardiovascular disease. Radiology 2010;257:541-8. [Crossref] [PubMed]
- Htwe Y, Cham MD, Henschke CI, et al. Coronary artery calcification on low-dose computed tomography: comparison of Agatston and Ordinal Scores. Clin Imaging 2015;39:799-802. [Crossref] [PubMed]
- Hecht HS, de Siqueira ME, Cham M, et al. Low- vs. standard-dose coronary artery calcium scanning. Eur Heart J Cardiovasc Imaging 2015;16:358-63. [Crossref] [PubMed]
- Yankelevitz DF, Henschke CI, Yip R, et al. Secondhand tobacco smoke in never smokers is a significant risk factor for coronary artery calcification. JACC Cardiovasc Imaging 2013;6:651-7. [Crossref] [PubMed]
- Salvatore M, Margolies L, Kale M, et al. Breast density: comparison of chest CT with mammography. Radiology 2014;270:67-73. [Crossref] [PubMed]
- Lung Cancer Progress Review Group Report 2001. National Cancer Institute. Chantilly Virginia. August 2001. Available online: https://searchworks.stanford.edu/view/8141183. Accessed April 20, 2016.
- Olsen LA, Aisner D, McGinnis JM, editors. The Learning Healthcare System: Workshop Summary of the Institute of Medicine Roundtable on Evidence-based Medicine. Washington DC: National Academy Press (US), 2007:4-10.
- Aberle DR, Black WC, Goldin JG, et al. (2003) Contemporary screening for the detection of lung cancer protocol [NLST], 10 May 2002. American College of Radiology Imaging Network (ACRIN sharp6654). Available online: http://www.acrin.org/6654_protocol.aspx. Accessed February 13, 2015.
- National Lung Screening Trial Research Team, Aberle DR, Berg CD, et al. The National Lung Screening Trial: Overview and Study Design. Radiology 2011;258:243-53. [Crossref] [PubMed]
- Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Prorok PC, Andriole GL, Bresalier RS, et al. Design of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Control Clin Trials 2000;21:273S-309S. [Crossref] [PubMed]
- Prorok PC, Marcus PM. Cancer screening trials: nuts and bolts. Semin Oncol 2010;37:216-23. [Crossref] [PubMed]
- Connor RJ, Eng D, Prorok PC. Issues in the mortality analysis of randomized controlled trials for cancer screening. Controlled Clin Trials 1994;15:81-99. [Crossref] [PubMed]
- Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med 2000;342:1878-86. [Crossref] [PubMed]
- Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 2000;342:1887-92. [Crossref] [PubMed]
- Olsen O, Gotzsche PC. Cochrane review of screening for breast cancer with mammography. Lancet 2001;358:1340-2. [Crossref] [PubMed]
- Miettinen OS, Henschke CI, Pasmantier MW, et al. Mammographic screening: No reliable supporting evidence? Lancet 2002;359:404-5. [Crossref] [PubMed]
- Miettinen OS, Yankelevitz DF, Henschke CI. Evaluation of screening for a cancer: annotated catechism of the Gold Standard creed. J Eval Clin Pract 2003;9:145-50. [Crossref] [PubMed]
- I-ELCAP Investigators. An Update of CT Screening for Lung Cancer. Semin Ultrasound CT MR 2005;26:348-56. [Crossref] [PubMed]
- Hanley JA. Analysis of mortality data from cancer screening studies: looking in the right window. Epidemiology 2005;16:786-90. [Crossref] [PubMed]
- Henschke CI, Boffetta P, Gorlova OY, et al. Assessment of Lung-cancer Mortality Reduction from CT Screening. Lung Cancer 2011;71:328-32. [Crossref] [PubMed]
- Foy M, Yip R, Chen X, et al. Modeling the mortality reduction due to CT screening for lung cancer. Cancer 2011;117:2703-8. [Crossref] [PubMed]
- Screening for lung cancer. United States Preventive Services Task Force. Available online: http://www.uspreventiveservicestaskforce.org/uspstf/uspslung.htm. Accessed February 13, 2015.
- Yankelevitz DF, Smith JP. Understanding the core result of the National Lung Screening Trial. N Engl J Med 2013;368:1460-1. [Crossref] [PubMed]


